Playlist
Show Playlist
Hide Playlist
Tubulointerstitial Pathology
-
Slides TubulointerstitialDisease RenalPathology.pdf
-
Download Lecture Overview
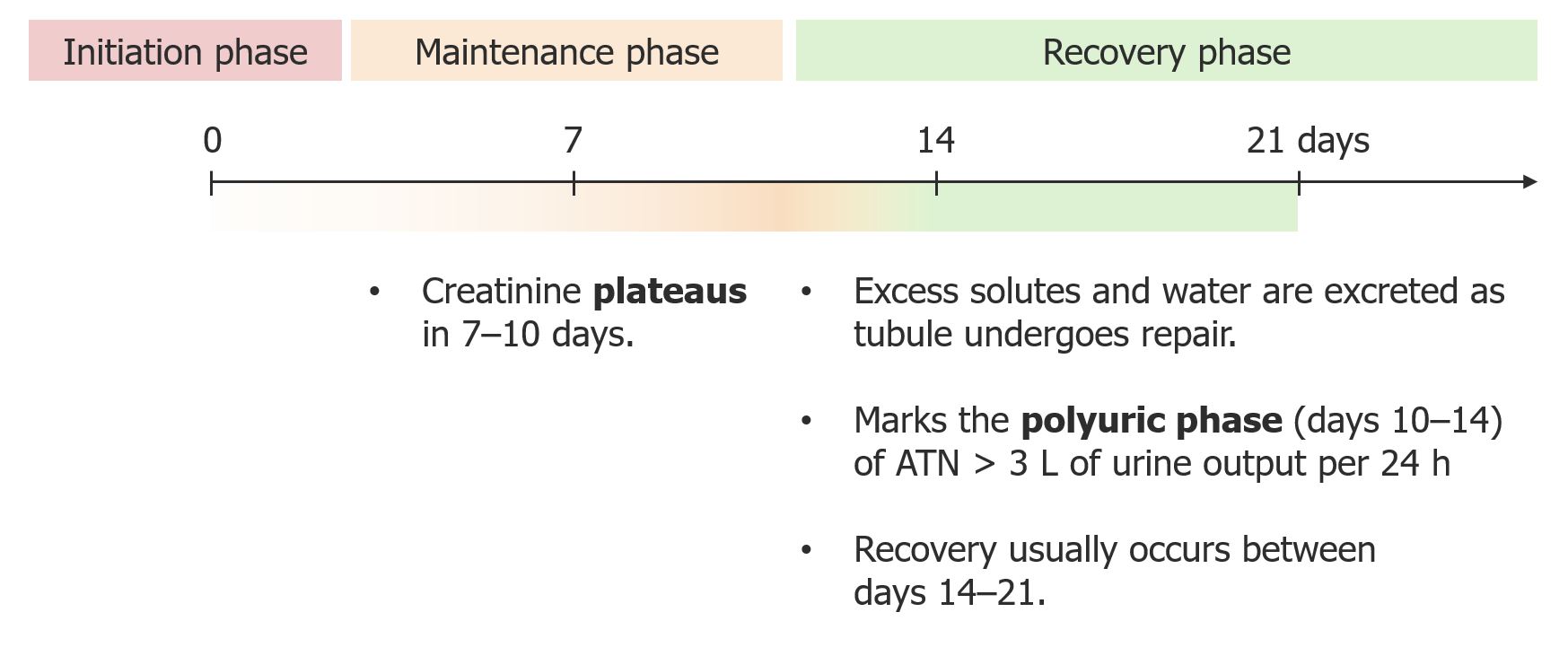
00:01 In this lecture series, we will move away from glomerular damage and take a look at other parts of the kidney in which our pathology is relevant. 00:13 Now, the first thing that you wanna do here is well, anatomically locate yourself and this would be tubulointerstitial disease. 00:22 So this is not dealing with the glomerulus, this is dealing with the tubules but keep in mind though, oftentimes, in order for you to cause damage to the tubule, you’ll have to pass through the glomerulus. 00:35 We call this acute kidney injury, AKI, acute kidney injury. 00:41 Keep this separate from RPGN that we talked about and later on at some point when we go down to chronic renal failure, well, we will then highlight as to what becomes important there. 00:53 So what kind of issues do you wanna keep in mind where the kidney obviously and got hurt in acute nature and by acute, what does that actually mean in reference to its timeline? Clinical pathologic process of acute renal failure, some of you have heard of it as such presenting as oliguria and you must know that oliguria refers to less than 400 milliliters of urine being produced in a day and one of the most common causes of acute kidney injury would therefore be acute tubular necrosis. 01:24 Now, necrosis to you should mean that the particular tissue is not receiving oxygen. 01:30 So therefore, one of the most common causes of acute tubular necrosis in fact will be ischemia. 01:37 We’ll take a look at ischemic ATN, nephrotoxicity, meaning to say that endogenously, there are certain substances that are being released maybe due to crush injury, and as so therefore, releasing myoglobin resulting in damage to the kidney in an acute nature. 01:54 Hemoglobin here, you might be thinking about what’s known as intravascular hemolysis, for example, paroxysmal nocturnal hemoglobinuria in which upon destruction of the RBC within the vasculature is then going to release the hemoglobin and this hemoglobin as it passes through and filters through the glomerulus may then cause damage and result in acute kidney injury. 02:15 Light chains, here, we’re thinking about monoclonal gammopathies including your well, multiple myeloma and company in which kappa/lambda chains may then cause not only damage to the glomerulus but may also cause damage to the tubules and then bilirubin and remember that you should normally have urobilinogen in your kidney so that you can give it that beautiful golden yellow color of a urine that you’re all so familiar with or you might then have conjugated bilirubin maybe due to hepatitis. 02:50 We talked about that in hepatobiliary. 02:52 Or exogenous type of damage that’s taking place to the kidney resulting in acute kidney injury. 02:58 Aminoglycosides, the antibiotics notorious for always making sure that the renal function is normal prior to administration. 03:07 Heavy metals, lead poisoning, resulting in lead nephropathy, sepsis, always worried about renal failure. 03:15 Other causes including volume depletion, urinary obstruction, RPGN, and perhaps even acute interstitial nephritis, AIN, but of all of the ideologies here of acute kidney injury, ischemic would be the most common. 03:30 Now, acute kidney injury, what are you looking for? Well, we’ll go through different phases here. 03:37 And remember, this is acute which means that the patient if all goes well and is receiving proper treatment should be able to recover the kidneys, you hear what I just said? So this is not chronic renal failure. 03:51 Chronic renal failure, now that’s a point of no return and for the most part, that patient, it’s just inevitable that he or she is going to then be placed on dialysis, correct? But then here, if it’s acute, we’ll go through different phases when the time is right in which at first, it very much behaves like a dead kidney. 04:11 Then, well go through maintenance phase and we’ll call something, we’ll call a phase in which regeneration’s taking place as being recovery. 04:20 At first, you’ll have hypertension just like you would with the chronic renal failure. 04:25 What does that mean? This means that you’re not able to properly filter your plasma, and so therefore, you are then holding on to fluid. 04:33 So your extracellular volume increases and maybe even perhaps angiotension II might play a role and with your patient with acute kidney injury early on is going to present with hypertension. 04:44 Next, in addition, acute kidney injury in the early phase, you are not able to properly filter, so therefore you are in a state of volume overload, excess water, and NaCl accumulating in your interstitium, edema. 05:01 Just like in chronic renal failure which is a very common cause of hyperkalemia, you are also going to find this early on and what you’re worried about with hyperkalemia is the fact that the heart might be affected, right? So meaning to say that now, your resting membrane potential is actually moving positive. 05:20 It’s becoming less negative and getting closer to threshold, be careful. 05:24 The pH here is the fact that now, you’re not able to properly hold on to the bicarbs, so therefore, metabolic acidosis or not able to properly produce your ammonia which takes place in the proximal convoluted tubule and these are some of the common places. 05:42 Think about your PCT, extremely metabolic active, remember that discussion. 05:47 So lots of sodium potassium pump activity, a lot of ATP and so therefore, for one of the common causes of acute kidney injury in fact is ischemia and you can only imagine that you’re not able to properly reabsorb the bicarb and so therefore very much behaves like an RTA type two. 06:04 However, here it’s different because you’re also creating a type of metabolic acidosis that would in fact be and an anion gap and that’s because of organic acids, so you want to be careful. 06:16 Remember that RTA type two is a metabolic acidosis but that is absolutely non-anion gap referring to, well, there’s no gap in anions with RTAs. 06:28 Here however there will be because of increased organic acid, that’s important. 06:32 What about erythropoietin? Well, just like chronic renal failure, take a look at this table. 06:37 This table kind of looks like what you'd expect to find in chronic renal failure. 06:41 Please be really careful. 06:42 Meaning to say that if you know that your patient is suffering form ischemia and you know it’s acute kidney injury, early on, it could look like chronic renal failure. 06:52 Here, erythropoietin is not present because of kidney damage, so therefore, you would expect your bone marrow to not function properly, look for a type of normocytic nonhemolytic type of anemia, erythroblast decreased stimulation. 07:05 To continue our discussion, along with acute kidney injury, you will also have bone issues. 07:12 We’ll talk more about this in chronic renal failure. 07:14 You might have problems where you’re not able to properly reabsorb calcium so you’ll have hypocalcemia, may result in what’s called as secondary hyperparathyroidism, and therefore, resulting in renal osteodystrophy but also at the fact that maybe the PTH can now properly work on your kidney, and so therefore, may result in renal osteodystrophy. 07:37 The phosphate would not be able to get rid of. 07:38 You have hyperphosphatemia. 07:40 The PTH as it just said here because you’re not able to properly reabsorb the calcium, result in secondary hyperparathyroidism and calcitriol. 07:49 Well, it’s not present because if the PCT has been destroyed early on, then you have decreased conversion because of decreased 1-alpha-hydroxylase activity resulting in osteomalacia type. 08:04 As far as the calcium’s concerned, it will be hypocalcemic and the reason for that as we said earlier is because there is going to be decreased production of calcitriol or maybe perhaps decreased functioning of your PTH. 08:17 Now, this is acute. 08:18 Management is directed towards correcting fluid overload, the hyperkalemia and signs of uremia. 08:26 So at first, everything that you’re doing here is very much paying attention to that table and the objective is to make sure that you take care of that hypertension, hyperkalemia, and those signs that we saw earlier. 08:40 Uremia referring to your signs, okay? So this will then be your hypocalcemia, secondary hypoparathyroidism, hyperphosphatemia, the anemia, the metabolic acidosis, and the declining mental status.
About the Lecture
The lecture Tubulointerstitial Pathology by Carlo Raj, MD is from the course Tubulointerstitial Diseases.
Included Quiz Questions
What is the clinical definition of oliguria?
- < 0.4 L urine production per day
- < 300 mL urine per 12 hours
- < 600 mL urine production per day
- < 2 L urine production per day
- < 1 L urine production per day
Which of the following is NOT a common etiology of acute tubular necrosis?
- Volume overload
- Sepsis
- Heavy metal toxicity
- Intravascular hemolytic disease
- Drug-induced by nephrotoxic antibiotics
Which of the following would NOT be present in renal tubular acidosis type II?
- Anion gap > 16
- Serum pH < 7.5
- Urine pH ≤ 5.3
- Serum bicarbonate of 22 mmol/L
- Impaired bicarbonate resorption
Which of the following is NOT a common clinical manifestation of acute kidney injury?
- Hyperphosphaturia
- Edema
- Normocytic anemia
- Hyperkalemia
- Hypertension
What clinical manifestations of acute kidney injury should be addressed first in terms of management?
- Hyperkalemia
- Hypocalcemia
- Secondary hyperparathyroidism
- Hypernatremia
- Hyperphosphatemia
Which of the following toxins causes acute kidney injury after crush accidents?
- Myoglobin
- Hemoglobin
- Bilirubin
- Light chains
- Heavy metals
Which of the following signs is associated with uremia?
- Declining mental status
- Hypercalcemia
- Hypophosphatemia
- Metabolic alkalosis
- Tinnitus
Which of the following clinical manifestations is associated with an acute kidney injury?
- Anemia
- Hypotension
- Metabolic alkalosis
- Hypokalemia
- Hypercalcemia
Why do patients with acute kidney injury undergo osteomalacia?
- The decreased conversion of 25-Vit D
- Volume overload
- Decreased tubular excretion of potassium
- Decreased filtration and excretion of phosphate
- Hyperphosphatemia
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Finally I understand the concept or the BUN/Cr ratio and the difference between prerenal and intrinsic
I don't like the use of acronyms when speaking because it is very distracting. Important content is all in the lecture which is a good thing, but I'd much rather use the pathoma videos for this topic.