Playlist
Show Playlist
Hide Playlist
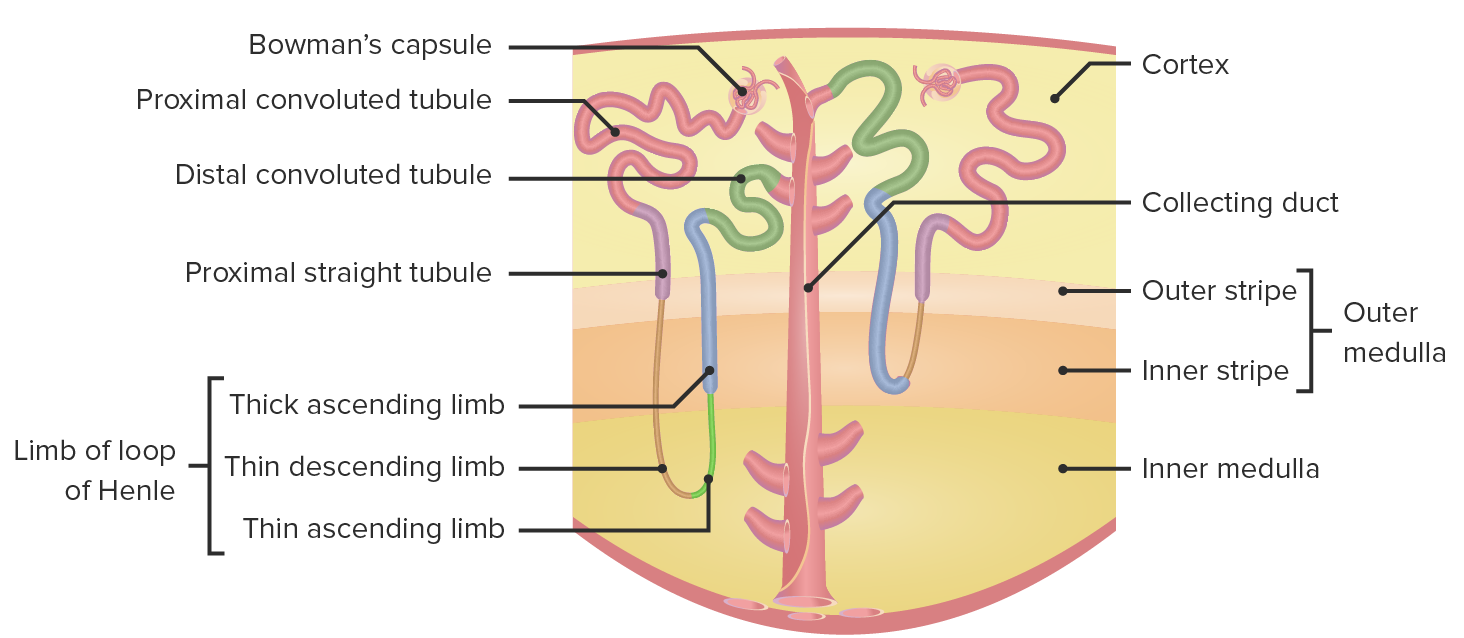
Tubular Transport by Nephron Segment
-
Slides NephronOverviewTubularTransportandTubularSecretion RenalPathology.pdf
-
Download Lecture Overview
00:00 Continuing with our discussion of our overview, we have A, B, C, D, E all set up here. 00:07 With A, B, C, D, E walking through this, we're going to put some of these together as you shall see. 00:13 And when we do, we will talk about those segments of the nephron in great detail so that you understand exactly the mechanism, the things that that part or that segment of the nephron is responsible for doing. We'll add in some pathology, put in some pharmacology, and obviously discuss a few adaptation issues as you shall see. Let’s take a look at segment A, which is the proximal convoluted tubule in great detail. Here, let me set up the picture for you. 00:43 You must understand, the lumen is the urine. You see that on your left. And then you have, what kind of a membrane is this? This membrane here, in fact, is your apical or luminal membrane. 00:55 And then you have your epithelial cell, which is your PCT. That’s exactly where we are. 01:00 And then you have the basolateral membrane which is then facing the what, please? The blood. Basolateral facing B, the blood. In other words, facing the interstitium. 01:09 Have you set this up clearly now? What are the mechanisms and what are the different processes that you’re already familiar with in the PCT? Ooh, lot of reabsorption taking place here at this point. 01:21 And by that we mean two-thirds of your sodium, potassium, chloride. You’re also taking up quite a bit of amino acids. How much of your glucose are you taking up? In previous discussions, we’ve had close to 100% of your glucose that’s being reabsorbed, haven’t we? Close to 100%, and that’s the one that I want us to, at this juncture, pay attention to. With this glucose, well, it can’t do it by itself. It requires a cotransporter, and this comes in the form of your sodium. 01:48 But in order for this to begin, you begin at the sodium potassium pump in the basolateral membrane. 01:54 You see the sodium potassium pump. And it is imperative that you pay attention to ATP. Why? I told you earlier that if, if the proximal convoluted tubule was undergoing a process of ischemia, lack of blood flow, you're not then delivering proper oxygen to the cell. And so therefore, the cell is not producing proper amounts of ATP because instead of aerobic, we’ll be travelling through anaerobic. And so therefore, you’re not feeding your biochemical processes of TCA nor electron transport chain. My point is this. If that ATP isn’t working as well then that cell may then perish. So those areas of the nephron that are extremely susceptible to hypoxia, PCT is one of them for the reason of that ATP. Now, continuing our discussion, as the sodium is being pumped out into the interstitium, how much sodium is left inside the cell? Not as much. 02:53 What have you created? You’ve created a gradient for sodium to rush in or be reabsorbed from your urine into the cell. Along with it, it may then bring in a number of substances in the form of symport, or we can do two things at the same time here. You can jump to another exchange, and this exchange that we’re seeing here is an antiport between sodium and hydrogen, right? But the basic premise, you begin at the pump. Always do that for me. And as long as it begins at the pump, then everything else makes sense in terms of reabsorption. 03:31 That has to be understood. Now, this path that we’re seeing here is transcellular, right? They’re moving through the cell. So that’s glucose. Let’s talk about bicarb. Bicarb coming from the blood filtering through, what kind of PH? You know this being an alkalotic, right? It is an alkalotic substance. 03:51 So bicarb is then filtered through. And tell me about bicarb. Most of it is reabsorbed. 80% is reabsorbed. 04:00 Indirectly or directly? Indirectly. As soon as you hear bicarb, physiologically, you’re thinking about which formula. You have your bicarb plus hydrogen and you have formation of your carbonic acid. 04:13 That does not require carbonic anhydrase. Is that clear? Where are all the different places where this formula you will see and have seen repetitively? Nephrology - renal system, gastroenterology - GI system, especially with what’s called this postprandial alkaline tide, and then up in the lungs, there once again, we’ll be dealing with bicarb, right? But as soon as you hear bicarb, you’re thinking about this formula right off the bat. 04:41 Automatically, it connects with hydrogen, you form your carbonic acid. Ah, now you have enzyme number one. “What does that mean, Dr. Raj?” Enzyme number one is carbonic anhydrase, number one. So you have this enzyme which will then take carbonic acid and you form your carbon dioxide and you form your water. Okay. Now, this is going to get readily reabsorbed into the epithelial cell. What are you going to do now? Carbonic anhydrase number two, do you see those bolden? Very important that you know this. Every second carbonic anhydrase, which is going to take that carbon dioxide and water, and form your carbonic acid, and spontaneously dissociates into hydrogen bicarb. Now, don’t get caught up in the details where you forget the objective. 05:28 What are we trying to do? Reabsorb bicarb. How much? 80%. Is that clear? Now, this bicarb that you are reabsorbing, is this newly synthesized or is this the reabsorbed type? Obviously, this is the recycling of bicarb. When you talk about newly synthesized bicarb, that will be done further in the collecting duct but not here. But at this point, we’re reabsorbing. 05:52 If you've understood this much, we're in good shape. Now, the only little clinical tag that I wish to bring to attention is the fact that what if you had a patient that was in high altitude. 06:02 So tell me about high altitude. Work with me here. Obviously, you know me well enough now where I can’t just go pass a particular segment or piece of information and just go through with the basics. No, no, no, no. This is medicine, people. So I want to go into high altitude. 06:19 If you go with the high altitude, what happens to your environment? You’re beyond air. 06:23 Beautiful up here, beautiful. Go to Rockies, huh? Go to Alps. I don’t know. Whatever. 06:28 There you are. You're looking at the landscape. It’s so pretty up here. But what happens with barometric pressure? It drops. Barometric pressure drops. Normally, at sea level, you’ve memorized 760 mmHg. And when you go into high altitude, the barometric pressure drops. 06:43 Maybe it drops down to 250. Oh, that’s really bad. So you’re taking the air here. 06:49 Okay. But once again, the barometric pressure is decreased. You continue forward and you travel through your trachea, down through your alveoli and such. 06:58 And eventually, well, guess what? Your barometric pressure is decreased. And so therefore, how is the body going to respond? How is the body going to respond? [panting sound]. 07:08 That’s not a panic attack. That’s me in high altitude, okay? If you’re having panic attack right now, take a brown paper bag. Breathe with me. But anyhow, high altitude, breathing really quick, breathing really quick, what happens to carbon dioxide? You’re blowing it off, blowing it off, blowing it off. Where am I? High altitude. You’re blowing off your carbon dioxide, what happens to your pH? Increases, right? What’s that called? Respiratory, respiratory alkalosis. 07:35 So therefore, what must you do in the kidneys days later in which you can compensate? What must you do down in the kidneys, here we go. This is where the clinical correlation's taking place. This is where the beauty of everything that you’re learning comes into play. 07:49 Work with it. So the kidney, days later, is going to compensate by doing what? Getting rid of bicarb. 07:56 Why? Because you're in a state of respiratory alkalosis. Why? Because you’re in a high altitude. 08:01 And what does that mean? Oh, decreased barometric pressure. The body wants to then breathe more obviously. Are we clear? So you’re trying to get rid of the bicarb, aren’t you? But let’s say that your patient doesn’t get rid of the bicarb quick enough. We have acute high-altitude sickness. So give me a drug that you know of that inhibits carbonic anhydrase. 08:21 Acetazolamide, okay? So acetazolamide inhibits our carbonic anhydrase. If you do look, then where is my bicarb? It’s stuck in the urine and you’re facilitating the compensatory mechanism of the kidney in a patient that has respiratory alkalosis. So therefore, now we’re good. 08:42 I’m giving you clinical correlations so that you clearly see the application and you’re not just sitting there and memorizing it. Now you think PCT, okay, good. You’re clear. You give yourself a little bit of a drug and put yourself in a situation, pathologically, physiologically, things will stick. 08:58 Let’s continue. What about the descending? Well, as we continue down the descending, what’s happening to water? It’s being reabsorbed, is it not? Of course, it is. As water is coming out, then what remains within the urine? It’s becoming more hypertonic. By the time you come to loop of Henle, naturally speaking, naturally speaking, without any influence of the hormone, listen to this statement so that you do not get this question wrong. Without the influence of a single hormone, what would be that region of the nephron that is most hypertonic, without the influence of a hormone? Obviously, the medullary loop of Henle because water is being reabsorbed. Nephron, the urine has electrolytes in it, solute. 09:46 So by the time you come to the actual loop, you’ll find it to be quite hypertonic but without the influence of any hormone. Why did I keep saying no influence of that hormone? Because if there was influence of hormone such as ADH, then the collecting duct would also be quite hypertonic. Are we clear? But at this point, we’re at the loop. So passively reabsorbs water, where am I? Coming down the descending limb, impermeable to solute, we did talk about that, hence hypertonicity. Now, we go to – look where you are – thick ascending limb. 10:20 First and foremost, thick ascending limb, that box that you’re seeing is the most important component of the thick ascending limb. Once again, clinical correlation. First and foremost, sodium potassium two chloride. Let’s set up the picture. The urine on the left, epithelial cell in the middle. What epithelial cell? Thick ascending limb. And on the right is your blood or interstitium. Okay. And we have a symport of three substances. 10:47 What does symport mean? Same direction, movement. The three substances, sodium, potassium, stop there. What are those in terms of charges? Cations, right? Well, isn’t the body about homeostasis and maintaining balance? Yes. Well, you have two cations. What must you then have to balance out the cations? How about a couple of anions? Ah, welcome to two chloride. Are we clear? So you have sodium potassium two chloride. That creates the balance that you require. 11:17 This is a symport. Now, this would be another area that is extremely susceptible to hypoxia because it’s very much dependent on that sodium potassium ATPase pump. So the pump is removing the sodium. It’s putting the potassium back into the cell. Stop there. Why? Because this potassium – pay attention – that potassium is being pumped back into the cell. 11:40 Potassium is also being brought in by the symport. And as you know, where do you find more potassium to begin with, ICF or ECF? Answer, I-C-F. So, if there’s already so much potassium in the ICF and you’re putting more in there, at some point, the potassium wants to do what? Explode. 12:02 It wants to come out and it does. That potassium, and we’ve talked about this in physiology, if you haven’t understood it, understand it now, which is not shown here but that potassium may then back-leak. It may then back-leak into the urine. You’ve heard of back-leak, haven’t you? And so, that back-leak of potassium back into the urine will then facilitate the reabsorption paracellularly. What’s para mean? Between the cells. You see that big, green epithelial cell? And then, you have another epithelial cell? And you have a space there? That’s paracellular. 12:39 So that potassium with back-leak will then force other cations including magnesium and some of that calcium to then get reabsorbed through the paracellular route. You want to know that. 12:51 You want to know the concept of paracellular or you want to know the concept of back-leak, and all because of too much potassium inside the cell. Interesting things? Sure. Are we quite done? No. 13:00 That’s sodium potassium two chloride. Give me a diuretic, give me a drug in which it inhibits that particular symport. It’s called loop diuretic, furosemide. That loop diuretic, as you know, one other point that I wish to make too, is that loop diuretic, we’ll talk about this coming up, a loop diuretic will not reach the sodium potassium two chloride through the glomerulus. 13:22 Think about what I just said. A loop diuretic does not exert its effect or action by being filtered, and then making it into the thick ascending limb. It doesn’t work like that, ladies and gentlemen. 13:35 The loop diuretic is going to work by, from the blood, the plasma, it’s going to get secreted with the help of, well, transporters. That’s important. Then, it will then work on the sodium potassium two chloride to do what? What are you trying to do? Loop diuretic. 13:52 Well, who’s your patient? Maybe he has pulmonary edema secondary to congestive heart failure. 13:57 What might you want to do to get rid of that fluid? A loop diuretic, huh? So there’s ease of breathing. 14:03 Okay. But the problem is this. When there’s loop diuretic, what are you going to lose? Everything, everything. You’ll lose sodium potassium two chloride and you’ll lose all your calcium. 14:12 Not good. So be careful. And so, you have to monitor specifically which electrolyte? That goes back to your basics. What’s the most important electrolyte that is responsible for maintaining resting membrane potential? It’s called potassium. Potassium is the most important electrolyte for maintaining resting membrane potential. Now, with the loop diuretic, what’s going to happen? There goes the potassium. Bye-bye, potassium. You’re flushing it down the toilet. So therefore, you start thinking about maybe giving your patient a potassium-sparing drug. So potassium has to be quite monitored when you’re using a drug like a loop. 14:50 We’ll talk more about that later. And then finally, there is a disease here, a pathology that will knock out the sodium potassium two chloride. And the name of that disease, we’ll talk about later. 14:59 Coming up. It’s called Bartter. All right. So we have two major. We have Gitelman and we have Bartter. 15:04 Now, Bartter, it’ll be the fact that it behaves like a loop. You haven’t heard of that before. That’s okay. 15:09 Bartter. Upcoming. Important. Couple of genes that we have to talk about that you may or may not be familiar with. But you'll hear it here first. Let’s continue. Here’s a back-leak. Why? Potassium being accumulated in your cell excessively. At some point, it backs into the urine. 15:29 Therefore, bringing about paracellular reabsorption of magnesium, calcium. It’ll be best, in terms of learning, to predict as to what’s going to happen by closing our eyes and conceptualizing. 15:40 Then later on, we take a look at the picture or the text, it’ll make sense and it’s coming together like that. Now, we get into the distal convoluted tubule, okay? Please leave PCT behind. 15:55 Our discussion quickly went through thick ascending limb and now we’re into distal convoluted tubule. 16:01 As soon as you hear this, the number one hormone that should come to mind, PTH. 16:07 Set up the picture again? Are we quite clear? Urine, left side, lumen. What’s in the middle? Epithelial side. What’s in the right side? The interstitium and the blood. Okay. What is PTH responsible for here specifically in the distal convoluted tubule? Only, only reabsorption of calcium. 16:26 Only. Why do I keep saying only? Because PTH also does what? It flushes phosphate down the toilet normally and physiologically. That is not taking place here. The PTH, as you’ve learned, and its effect of inhibiting the reabsorption of phosphate will be in the PCT. That’s important. 16:49 And the last bit of component of PTH and its effect of activating whom? Calcium, well, calcitriol. Another important calcium homeostatic hormone, vitamin D. That’s through activating, that enzyme is, you tell me, good, 1-alpha-hydroxylase. But that would not be here. 17:11 Once again, that’s in the PCT. So let’s just talk about PTH and its receptor, and as to how you are going to bring about calcium reabsorption. Let's begin at the top with the sodium potassium pump. 17:22 There it is. Removing sodium. What happens to sodium concentration within the cell? It decreases. 17:27 Then you have a symport mechanism. And here’s sodium and chloride. Approximately 25% of your sodium only is being reabsorbed. Majority of it? The majority of it was already done in your PCT. 17:39 So this takes care of a little bit more sodium. Chloride is going to come out. And then, you take a look at the basolateral membrane, please. You have an antiport that you're seeing there. 17:48 Then with the help of PTH, it will then reabsorb my calcium. It’s important that you pay attention there. 17:54 Okay now, let me give you a couple of pathologies. What if you have hyperparathyroidism? Hyperparathyroidism, primary, not secondary, primary. That means that, think about your parathyroids around your thyroid gland. That’s four of them. And it’s an adenoma producing too much parathyroid hormone. Welcome to primary hyperparathyroidism. Tell me about your calcium levels. 18:18 It'll work on the distal convoluted tubule to reabsorb calcium. Welcome to hypercalcemia. 18:24 And if it's hyperparathyroidism, primary type, what is it going to do to phosphate levels in the PCT? It will further inhibit the reabsorption. Welcome to hypophosphatemia. And last little thing that you want to keep in mind with PTH is always check for renal function. We’ll talk more about that later. But right now though, I’m giving you one example for hyperparathyroidism. 18:49 The only other thing that I wish to bring to attention is that receptor, and by chemistry, by chemistry, we talked about a receptor known as G protein. You know about Gs, and Gi, and Gq. You tell me. 19:04 I’ll tell you why this is so important. You tell me which G protein does PTH work through. 19:10 It’s called Gs. Really? Mm-hmm. What if you find a pathology in which you’d find decreased levels of cyclic AMP in the urine? Wow! How do you relate all these together? Gs. What’s the number one letter you’re thinking about Gs? A-A-A-A, adenylyl cyclase. You convert your ATP into cyclic AMP and your protein kinase A. You think of Gs, you think of A, right? So you have your adenylyl cyclase and ATP, and cyclic AMP, and you have your protein kinase A. Are we good? So as long as you have PTH working properly, you should find just enough cyclic AMP in the urine to make sure that you're properly functioning. If it's primary hyperparathyroidism, obviously, you'd find too much cyclic AMP. Would you give me a name of a pathology where the receptor isn't working? I didn't even know such a condition existed. Yes, you did. Yes, you did because now you call it knuckle knuckle dimple dimple. What? Now unbelievably, this patient, short stature, fourth and fifth digit, the knuckle which is a metacarpophalangeal, you don't have a knuckle. 20:27 They're dimpled. It's inverted. Why? It's crazy. But that's how this patient is going to present. 20:34 A short patient, knuckle knuckle dimple dimple, fourth and fifth digit, their knuckles are not present. 20:41 They're not properly formed. And the receptor isn't working properly, so you find decreased levels of cyclic AMP in the urine. Welcome to pseudohyperparathyroidism. Wow! Dr. Raj, I had no idea that all this stuff could be derived by looking at a simple picture like this. Yes, you did. 20:58 You just never applied yourself. So now, we take a look at our collecting duct. In our collecting duct, these are things that, once again, physiologically are important for us. We spend quite a bit of time with this. Let's put all these together. Once again, set up the picture. 21:14 We have the lumen and the urine. We have the epithelial cell. And we have the interstitium, correct? Reabsorption means what? From the urine out into the blood. Secretion means you’re going into the urine. Clear? Next, when we do our collecting duct, take a look where we are. 21:29 We have two major cells. We have a principal cell, intercalated cell. Your emphasis and focus should be principally, pun intended, on the principal cell. Now, the hormone that we’re going to bring in here will be aldosterone. Why? Maybe your patient had decreased blood pressure. 21:47 Maybe your patient had congestive heart failure. Are we clear about those? Decreased blood pressure, decreased perfusion to the renal artery. Here comes my renin. Ah, I kick off my RAA System. 21:58 Congestive heart failure, my heart is dead, and more of my plasma, my transudate is being hydrostatically pushed into the interstitium. Welcome to maybe pulmonary edema and dyspnea and such. If it’s right side, welcome to positive JVD and pitting edema. What’s my point? When this fluid has escaped the blood vessel and has gotten into an interstitium, well, how was the juxtaglomerular apparatus going to interpret this? Decreased effective circulating volume, right? So therefore, welcome to RAAS again. So here's my aldosterone. 22:34 and all this. If you've missed that discussion about CHF, cardiology, and then here, aldosterone comes in and it binds to the receptor. Where? Well, the receptor will be bound to, let’s say, on the basolateral membrane. Once it works upon that receptor which is then called, well, aldosterone receptor, and that’s important for you to understand because you can have what's known as aldosterone receptor antagonist. Give me the drug, spironolactone, clinical tag there. Stop. This aldosterone can do what with the sodium potassium pump? What is its main objective? To reabsorb sodium. So it will stimulate that pump, or on the luminal membrane or the apical membrane, that’s called epithelial sodium channel, eNaC, so to reabsorb sodium through there as well. Now, understand though, they will not have you differentiate between, well, which one doesn’t work more. That's a ridiculous question. 23:34 It doesn’t accomplish anything. Aldosterone will do everything in its power to reabsorb sodium. 23:40 Stop there. What else does aldosterone do? It works here to get rid of your potassium. 23:45 In other words, secrete on potassium. Clear? What's the third and final thing that aldosterone does? I want you to drop down to the intercalated cell. You see that? The intercalated cell. 23:57 That intercalated cell, I want you to focus upon. I need you to find hydrogen and that hydrogen is being secreted into the urine. Guess who does this. Aldosterone does. Let me give you a very common enough cause of secondary hypertension, in which upon imaging study of the adrenal, Let’s say a CT, you find a tumor within the adrenal cortex in which you're strictly producing only aldosterone. So this is not buffalo hump, moon face, it’s not Cushing's, strictly increase in hypertension or blood pressure, secondary type. This is Conn’s syndrome. I’ve mentioned this a few times because I want you to get in the habit of understanding your labs. If you have aldosterone in excess, specifically, what's my sodium level as a concept? Increased. Please give me a value. 24:52 Above 145, number one. Number two, if you have too much aldosterone, what happens to potassium? It’s being secreted out. Give me a number. Less than 3.5. So far, so good. Number three, hydrogen or too much aldosterone, you're secreting hydrogen into the urine. Tell me about the pH. 25:14 Alkalotic, increased. Are we good? If you're not, review that concept real quick. 25:20 In Addison’s, I would ask you to do this. With Addison’s, I want you to compare Conn’s with Addison’s. 25:27 In Addison's, you're deficient of aldosterone. Primary adrenal insufficiency. All the labs will be reversed. 25:36 Decreased sodium, hyperkalemia, decreased pH. You understand this? You’ve understood a bunch of pathologies. Let’s continue. Here as well, we have ADH, ADH receptors. 25:50 How many kidneys do you have? Oh, one. Two. Very good. V2 receptors. Why do we call these V? Because they're vasopressin. It's another name for ADH. Where else may ADH work? A name, vasopressin, V1, on your blood vessels, bringing about vasoconstriction. 26:09 Through V2, you're going to insert aquaporins. And if need be, what do you mean need be? I just ran through the desert. Oh, that's a lot of sweat. I’m losing a lot of fluid. I am losing more water than I am sodium. Dr. Raj, when I sweat, and I taste myself, I taste mighty good. What does that mean? I taste salty. Okay, fine. You like salt. That’s great. But understand, you’re losing more water. Clear? Okay. So if you're losing more water than salt, what is your plasma osmolarity, please? Good. Increased. 26:50 Are we good? Your plasma osmolarity is increased. Where are you now? Who’s going to detect this immediately? Who's going to detect this immediately? Hypothalamus. Hypothalamus. Through whom? Osmoreceptors. So you sweat so much, huh? And you’re losing that water. 27:09 The body wants to replenish it. Where is it going to get it from? The kidney. Kidney. 27:14 Are you understanding this? So who are you going to release? Who are you going to release? ADH, antidiuretic hormone. Here comes ADH to the rescue, at least initially. 27:24 And it works in the V2 receptors, puts in, inserts aquaporins. Were you going to reabsorb more water? Now, you tell me. On the side of the urine, be careful when you do such questions. 27:35 And if you're dealing with attendings and such in your CPC, you will differentiate between urine osmolarity and plasma osmolarity. Do that every single time. Here with ADH working, what kind of urine are you producing? Good. Concentrated hypertonic urine. Excellent. 27:55 So far, so good? This is the collecting duct issues here.
About the Lecture
The lecture Tubular Transport by Nephron Segment by Carlo Raj, MD is from the course Diseases of the Nephron.
Included Quiz Questions
Which of the following is not true regarding the transport at the proximal convoluted tubule?
- Reabsorption of almost 80% of bicarbonate occurs directly at the PCT.
- Reabsorption of almost 100% of glucose occurs at the PCT.
- Sodium-potassium ATP pump is affected during the ischemia of PCT.
- Reabsorption of almost 80% of bicarbonate occurs indirectly at the PCT.
- Carbonic anhydrase leads to the formation of carbon dioxide and water, which gets absorbed and converted into bicarbonate in the epithelial cell of the PCT.
In high altitude sickness, a drug is given in order to facilitate metabolic compensation. Which of the following statements is true?
- Acetazolamide inhibits carbonic anhydrase, that leads to the inhibition of bicarbonate formation.
- Acetazolamide stimulates carbonic anhydrase, that leads to the inhibition of bicarbonate formation.
- Acetazolamide inhibits carbonic anhydrase, that leads to the stimulation of bicarbonate formation.
- Acetaminophen inhibits carbonic anhydrase, that leads to the inhibition of bicarbonate formation.
- Acetaminophen stimulates carbonic anhydrase, that leads to the inhibition of bicarbonate formation.
What region of the nephron has the most hypertonic urine without the influence of a hormone?
- Medullary loop of Henle
- Cortical collecting duct
- Distal convoluted tubule
- Medullary collecting duct
- Cortical loop of Henle
Which drug is responsible for inhibiting the sodium, potassium, and chloride reabsorption in the thick ascending limb of the loop of Henle?
- Furosemide
- Famotidine
- Metolazone
- Spironolactone
- Chlorthalidone
Which of the following drugs could be given with a loop diuretic to keep the resting membrane potential intact?
- Spironolactone
- Chlorthalidone
- Metolazone
- Acetazolamide
- Acetaminophen
Which of the following facilitates paracellular reabsorption of magnesium and calcium in the thick ascending limb of the loop of Henle?
- Back-leak of K+
- Back-leak of Na+
- Back-leak of Cl-
- Back-leak of H+
- Back-leak of HCO3-
Which of the following is true regarding the effects of parathyroid hormone on the metabolism of calcium and phosphate?
- Reabsorption of calcium in the DCT, and inhibition of reabsorption of phosphate in the PCT
- Reabsorption of phosphate in the DCT, and inhibition of reabsorption of calcium in the PCT
- Reabsorption of calcium in the DCT, and reabsorption of phosphate in the PCT
- Reabsorption of calcium in the DCT, and stimulation of reabsorption of phosphate in the PCT
- Inhibition of reabsorption of calcium in the DCT, and inhibition of reabsorption of phosphate in the PCT
Which of the following statements is true regarding the activation of 1-alpha hydroxylase in the nephron?
- It is activated by the PTH in the proximal convoluted tubule.
- It is activated by the PTH in the distal convoluted tubule.
- It is activated by the PTH in the medullary collecting duct.
- It is activated by the PTH in the cortical collecting duct.
- It is activated by the PTH in the descending loop of Henle.
Which of the following changes usually occur in primary hyperparathyroidism?
- Hypercalcemia, hypophosphatemia
- Hypocalcemia, hypophosphatemia
- Hypercalcemia, hyerphosphatemia
- Hypocalcemia, hyperphosphatemia
- Hypernatremia, hypophosphatemia
Which of the following is part of the PTH receptor in the distal convoluted tubule?
- Gs
- Gi
- Gq
- Protein kinase A
- Protein kinase C
Which of the following statements is true regarding the function of aldosterone?
- Reabsorption of sodium, and secretion of potassium
- Reabsorption of potassium, and secretion of sodium
- Reabsorption of sodium, and secretion of phosphorus
- Reabsorption of water, and secretion of potassium
- Reabsorption of sodium, and secretion of chloride
Which of the following receptors is involved in the reabsorption of water by the antidiuretic hormone?
- V2 receptor of the principal cell
- V1 receptor of the principal cell
- Aquaporin in the intercalated cell
- V1 receptor of the blood vessel
- Aquaporin in the hypothalamus
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This is an excellent lecture that integrates other body systems and applies the effects to the kidneys. Understanding where and why all of the hormones act on the nephron was thoroughly and expertly explained. Very, very well done.
Most lectures about nephron segment is kind of boring. But I really like Dr. Raj's passionate and clear explanation, and the way he sophisticated getting knowledge connected with clinical application. It's the best nephron segment lecture ever.