Playlist
Show Playlist
Hide Playlist
Overview of Calcium Metabolism Disorders
-
Slides Hypercalcemia.pdf
-
Download Lecture Overview
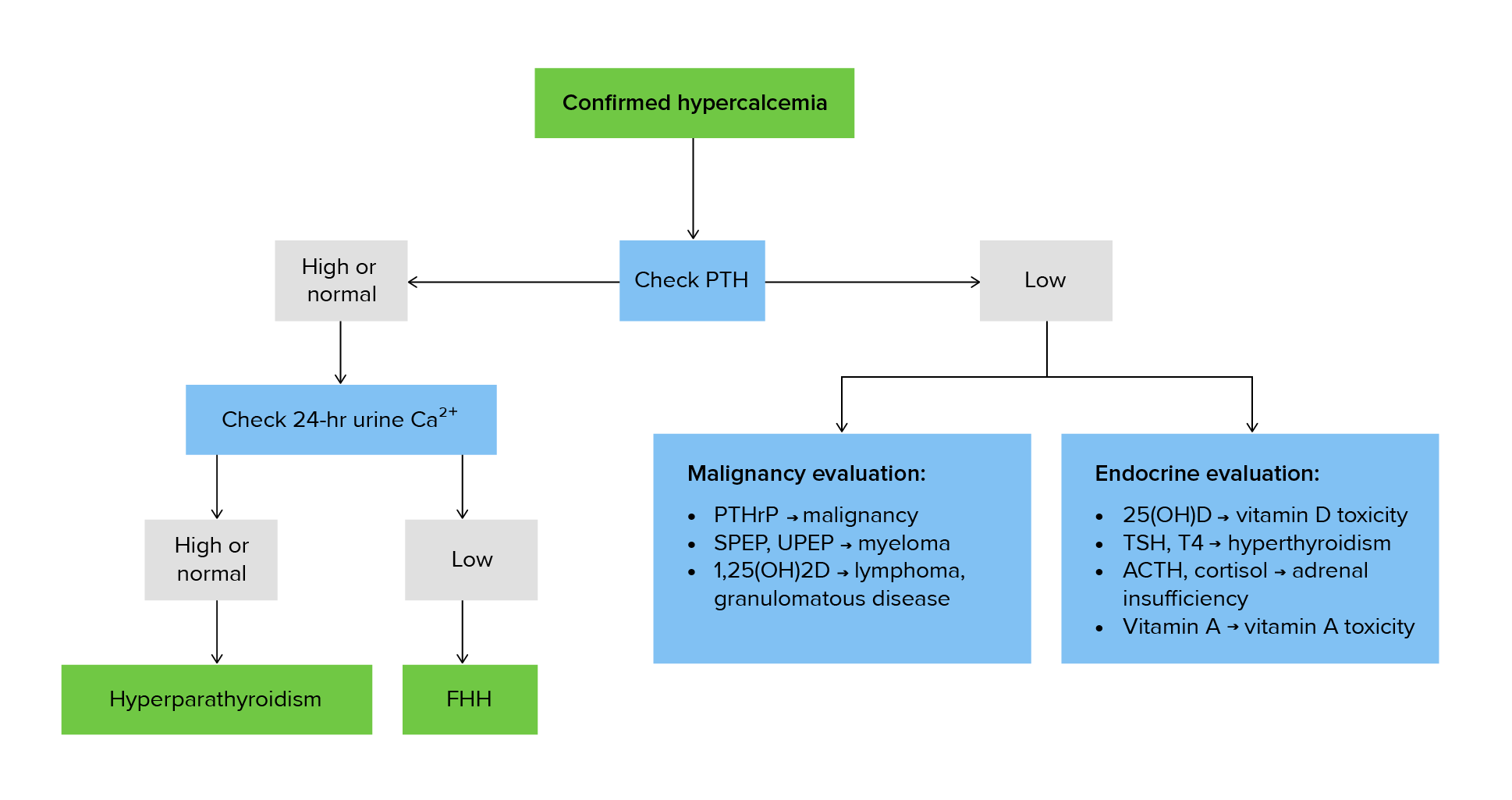
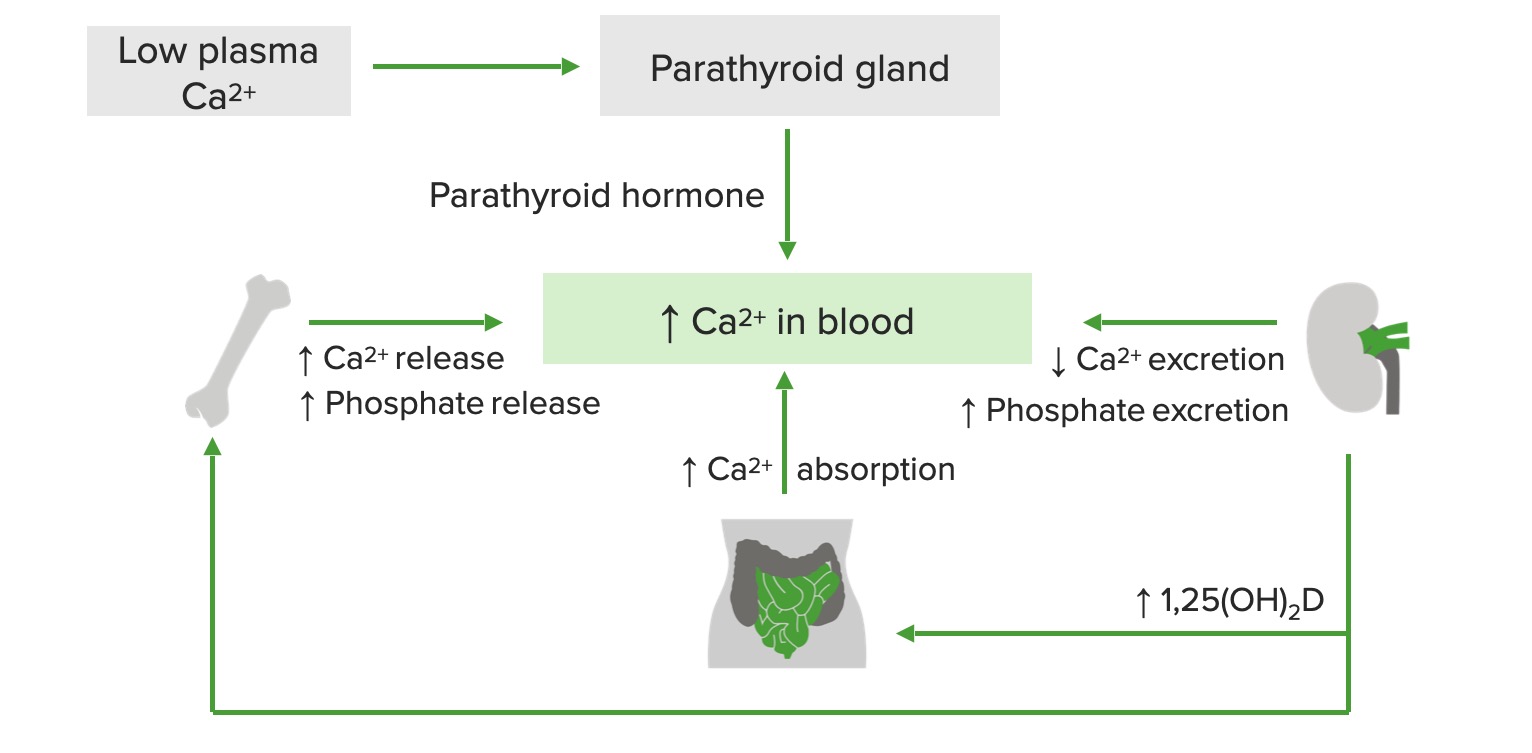
00:01 Our discussion here takes us into calcium metabolism overview. 00:05 Important that you know the foundation here so that we can get into the extremes of calcium. 00:12 What controls calcium? How important is calcium? Well, without calcium, we wouldn’t able to make proper bone; without the calcium, we have no signal transduction. 00:21 You know about IP3 and phospholipase C, you’ve heard of calcium calmodulin, calcium is all over the place. 00:28 Calcium, within the heart and also within your skeletal muscle, responsible to then bind to your troponin C bringing about muscle contraction, let it be the heart or it be the skeletal muscle. 00:40 Calcium, crucial for existence. 00:44 The bone itself is made up of calcium and phosphate, together we call this hydroxyapatite. 00:48 You also have magnesium who are all regulated and any time that there is a problem with calcium, things become a little interesting, don’t they? It’s important that you understand the places in our body where calcium is properly metabolized or controlled. 01:02 We’ll take a look at the bone and you remember kidney in nephrology. 01:05 Those will be the two big ones that we will be paying attention to. 01:08 Now, the hormones that are responsible for maintaining calcium metabolism include PTH. 01:14 So, for example, if for whatever reason, calcium levels have dropped, for example, most common cause of osteomalacia in the United States would be renal failure and if the kidneys die, then PTH goes along with it, meaning to say it’s not functioning. 01:30 You’re not able to properly activate your 1-alpha-hydroxylase, you do not have calcitriols so, therefore, your calcium levels will drop. 01:38 If the calcium levels will drop, then you can only expect that the PTH in the parathyroids will be releasing it resulting in what’s known as, eventually we’ll talk about, secondary hyperparathyroidism. 01:50 Vitamin D... 01:52 Vitamin D, from head to toe, and by that I mean, the different ways in which you can acquire vitamin D would be perhaps from the skin upon exposure to UV rays or you’re drinking vitamin D fortified dairy product. 02:03 When you do so, you’re taking in inactive vitamin D, all these is taken up by the liver or taken to the liver. 02:11 Here, it would be hydroxylated with 25. 02:14 This is the major circulating type or form of vitamin D which then eventually makes its way to the kidney where, with the help of PTH and 1-alpha-hydroxylase in the PCT, you activate your vitamin D… welcome to calcitriol. 02:28 Do not get your calcitriol confused with calcitonin. 02:32 Calcitonin does play a role with calcium metabolism, but in terms of its exact effect, we are not mentioning that here. 02:39 A lot of research in exactly as what’s occurring at least know that calcitonin does play a role in calcium homeostasis. 02:48 Calcitonin can be used as a tumor marker when you’re thinking about medullary cancer of the thyroid, your parafollicular C cells will be releasing your calcitonin. 02:57 Once again, do not confuse your calcitonin with calcitriol. 03:00 I’d like for you to take a look at the picture here and we have ECF as a very small percentage of actual calcium… ECF does. 03:09 So, where is majority of your calcium? Inside my bone. 03:14 Next, in order for you to form proper mineralized bone, you need to acquire both calcium and phosphate. 03:20 There would be constant exchange between the two of them. 03:22 It’s important for you to know that, remodelling is quite important for the bone. 03:26 Meaning to say that there is sufficient amount of bone breakdown, but at the same time, there is sufficient amount of replacement of that bone as well. 03:35 Hence, osteoclast and osteoblast play critical role with maintaining proper remodelling of the bone hence making it stronger and stronger and stronger. 03:44 Hence, what you recommend to a lady who has reached menopause at an approximate age of 50 is too oftentimes participate in weight bearing exercises. 03:55 Now, the exact mechanism is at this point eludes us, but we do know that weight bearing exercises promotes remodelling in a female who has hit menopause and at risk for osteoporosis. 04:09 From the food, on your right, you find that from the intestine with the help of vitamin D, we’re going to reabsorb that calcium, but in order for the vitamin D to work upon your intestine, it is important that you know that activation will take place down in the proximal convoluted tubule of your kidney. 04:28 Regulation of calcium by PTH. 04:29 So, what exactly is occurring here? Once again, the PTH is made by chief cells in the four parathyroid glands. 04:38 The inferior parathyroids is giving rise to and binds to the third pharyngeal pouch. 04:43 In addition to the inferior parathyroids giving rise by your third pharyngeal pouch, you also have the thymus. 04:50 And if you have a condition such as DiGeorge in which your third and fourth pharyngeal pouches are not working properly or not developed properly, you would not have the parathyroids that are responsible for calcium reabsorption, you can expect there to be hypocalcaemia. 05:04 When the serum ionized calcium levels are low, I gave an example such as renal failure resulting in osteomalacia. 05:11 With that vitamin D deficiency in an adult renal failure, you can expect your calcium levels to be low resulting in triggering your PTH to then increase. 05:19 We then call this secondary hypoparathyroidism. 05:22 This PTH, we’ll talk about this later in which it will then play a role in different organ systems, but any time, homeostatically, whenever calcium levels are low, the PTH is quick, quick to be released and when it does, it then plays a role with normal calcium metabolism. 05:40 Regulation of calcium by PTH and our discussion continues. 05:46 You must know that PTH works through a G-protein, this G-protein is known as your Gs and that, to you, should mean ATP cyclic AMP. 05:58 Where does PTH work to reabsorb calcium in the kidney? It works in the kidney in the distal convoluted tubule to reabsorb calcium. 06:06 The receptors for PTH for reabsorption, in fact, are in the DCT. 06:10 When PTH binds to the receptor, it will then increase the amount of cyclic AMP within your nephron. 06:16 Any time that you have a pathology in which these receptors for PTH aren’t working, namely pseudohypoparathyroidism, you would not find sufficient amounts of cyclic AMP within your urine. 06:31 Increased calcium reabsorption in the kidney is what PTH does; increases phosphate wasting. 06:36 In other words, in the kidney PTH does what? It flushes out the phosphate, the opposite effects in the kidney. 06:44 Also, in the PCT, PTH works on that enzyme that I have referred to a few times known as 1-alpha-hydroxylase adding the 25… adding to the 25 resulting in our product known as calcitriol or 1,25 dihydroxycholecalciferol. 07:03 Next, vitamin D, as you see-see in the illustration here, the red arrow, you see the increased of 1,25 vitamin D, that’s calcitriol. 07:14 Did you-Did you identify it? It works in the intestines so that it reabsorbs your calcium; it also works in the kidneys so that it reabsorbs calcium. 07:23 The overview of your calcium homeostasis and PTH we said will flush out the phosphate; that high phosphate levels promote PTH release. 07:35 Once again, if you have hyperphosphataemia, it will release PTH so that the PTH can flush out the phosphate in your PCT. 07:46 Two major functions of PTH in the PCT - Activate 1-alpha-hydroxylase and to flush out the phosphate. 07:53 One major function of the PTH in the DCT and that is to reabsorb your calcium, if you remember from physio. 07:59 Ultimately, the renal calcium-calcium handling by PTH in the nephron would be the following. 08:07 I want you to focus upon the DCT, distal convoluted tubule, we have a drug here that works known as thiazides and we have a hormone here that works. 08:19 Both of these products either form or your PTH in physio will work to reabsorb your calcium. 08:26 Yes, thiazides remove calcium out of your nephron, do not ever forget that, that’s important.
About the Lecture
The lecture Overview of Calcium Metabolism Disorders by Carlo Raj, MD is from the course Parathyroid Gland Disorders.
Included Quiz Questions
What correctly matches the hormone and its effect on calcium?
- Calcitonin—decreases serum calcium
- PTH—decreases serum calcium
- PTH—increases serum phosphate
- Magnesium—increases serum calcium
- Vitamin D—decreases calcium absorption
What is associated with drastically increased calcitonin?
- Medullary cancer of the thyroid
- Melanoma
- Squamous cell carcinoma
- Small cell lung cancer
- Colorectal cancer
Which cells synthesize PTH?
- Chief cells of the parathyroid
- Oxyphil cells of the parathyroid
- Parafollicular cells of the thyroid
- The proximal convoluted tubule of the kidney
- Juxtaglomerular apparatus of the kidney
A patient presents with DiGeorge syndrome. Which embryologic structures, responsible for forming the parathyroid glands, failed to form in this disease?
- 3rd and 4th pharyngeal pouch
- Rathke's pouch
- Branchial cleft
- Pleuroperitoneal folds
- The dorsal and ventral bud
What is NOT an effect of PTH?
- Decreased phosphate absorption in the intestine
- Increased intestinal absorption of calcium
- Increased bone resorption
- Increased phosphate excretion in the kidney
- Stimulates activation of Vitamin D
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
It is satisfying especially if you read before about the effects of PTH.
He is good But honestly its really hard to follow along with what he is saying (even after prereading before the video). Sometimes I feel he jumps around concepts. Mentions something and you thing what he says next its relevant to the previous things and no.
Overall great but wish they had more info on Calcitonin action