Playlist
Show Playlist
Hide Playlist
Vasculitis: Introduction
-
I Rheumatology 05 Vasculitis.pdf
-
Download Lecture Overview
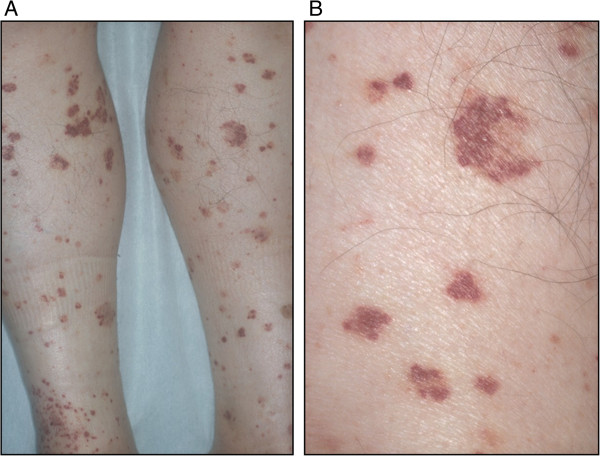
00:01 Hello. Welcome to our discussion of vasculitis. 00:04 In my opinion, the best approach to take a look at vasculitis would be to organize it into large, middle, and small vessel vasculitities. 00:11 Let’s have a look. 00:14 So vasculitis itself—I want you to step back for a second and think of what that actually means. 00:21 Whatever blood vessel that we choose as we go through the differentials here, let it be large, middle, or small vessel, well that vessel is undergoing inflammation. Vasculitis. 00:33 Well depending as to which blood vessel we’re going to focus upon will then depend on what kind of clinical manifestations that the patient’s presenting with. Correct? Now for example, let’s say that there’s inflammation taking place of a large blood vessel such as the branches of the arch of aorta. 00:51 You have pretty massive issues then. For example, Takayasu, we’ll talk about. 00:55 What if it was a middle-sized blood vessel such as a mesenteric artery or maybe the renal artery and such, and then inflammation is bringing about occlusion, and then you would then have what? End organ damage, wouldn’t you? Or maybe you’re talking about cutaneous blood vessels that are undergoing inflammatory process and how would that patient present? Well then obviously you’re looking at “rash.” The best way to think about this; however, is also the following: it could be idiopathic or connective tissue disease associations. 01:29 So for example, let’s say that we’re discussing polymyalgia rheumatica and you have an older lady who, all of a sudden, starts complaining about pain in the jaw or maybe perhaps up here in the temporal region. 01:45 The combination of the 2, giant cell arteritis overlapping with polymyalgia rheumatica, where your patient might then be having issues in the neck and the upper shoulders and such. 01:57 Infectious? Often times there might be an antecedent prodrome of a viral infection following the vasculitis. 02:07 Keep that in mind. And maybe perhaps malignant as well. 02:12 As I said, the method that I like using here is to organize your blood vessel issues. 02:17 For the large vessel. With that said, let’s begin with our first discussion, Takayasu. 02:23 Who is this patient walking through the door? So a young lady, younger than the age of 40, and she’s of Asian descent most commonly. 02:33 Now which large blood vessel are we referring to? Well here, we’ll talk about the branches of the aorta. 02:41 Our next patient, with large vessel disease, will be giant cell. 02:45 Under giant cell arteritis, we’ll be talking about the branches of the temporal artery; and with this patient, older lady most commonly, that if left untreated, then the ophthalmic branch might then undergo granulomatous changes resulting in blindness if left untreated—we’ll talk about. 03:05 Medium vessel disease—we’ll take a look at polyarteritis nodosa. 03:09 Want you to think about the GI and the kidney. As soon as you think about PAN, I want you to get in the habit of what you’re looking for in your patient. 03:17 Therefore, you’re looking for abdominal pain and you’re looking for maybe hematuria because of renal blood vessels are being affected. 03:25 Be careful here under medium vessel. 03:28 Technically speaking, some of these blood vessel pathologies could affect medium and small blood vessels, so do not get trapped or do not contain yourself or put yourself into a box thinking, “Oh, well mesenteric artery versus a capillary—that must be small vessel.” No, you’re going to be paying attention to the most common presentation. 03:48 For example, Buer-is what this says versus Ber, you pronounce it pretty much the same. Buerger or maybe Buerger. 04:03 What I’m saying is, to a layman, it sounds exactly the same. Buerger and Berger. 04:08 Two different pathologies all together. 04:11 What is the most common nephritis in the world? Berger—Ber. 04:17 That is not our topic. Our topic is vasculitities. 04:22 This is Buer—a better name for this would be thrombangitis obliterans and I’ll give you the common presentation where most likely a male, who’s a smoker, and the little blood vessels in the foot may be perhaps be affected and therefore gangrene might set in. 04:39 <i>Another form of medium vessel vasculitis is Kawasaki disease.</i> <i>Its diagnosis requires a fever lasting at least 5 days</i> <i>without another explanation, and at least 4 out of 5 of the following symptoms:</i> <i>first, bilateral conjunctival infection;</i> <i>second, oral mucosal changes like fissured lips,</i> <i>strawberry tongue or something similar;</i> <i>third, a rash; fourth, cervical lymphadenopathy;</i> <i>and fifth, erythema of the palms or soles or other extremity changes.</i> <i>Additionally, Kawasaki disease is the one exception to giving aspirin to children.</i> And under small vessel, we’ll divide this into ANCA positive or non-ANCA small vessel disease. 05:27 Of course under ANCA, the prototype often used for something that used to be cANCA positive which is now called PR3-ANCA or proteinase 3-ANCA. 05:37 It used to be called Wegener, but now we call it granulomatosis with polyangiitis, but you know what I’m trying to get at. 05:45 And then under non-ANCA, we’ll take a look at Henoch-Schönlein purpura. 05:49 Another name for this, and properly and correctly, is called IgA vasculitis. 05:56 Also take a look at quickly cutaneous leukocytoclastic angiitis and also essential mixed cryoglobulinemia.
About the Lecture
The lecture Vasculitis: Introduction by Carlo Raj, MD is from the course Vasculitis: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is a large vessel vasculitis?
- Takayasu arteritis
- Polyarteritis nodosa
- Buerger disease
- Henoch-Schönlein purpura
- Cutaneous leukocytoclastic angiitis
Which of the following is an IgA vasculitis?
- Henoch-Schönlein purpura,
- Polyarteritis nodosa
- Takayasu arteritis
- Giant-cell arteritis
- Buerger disease
What is the most serious complication of giant cell arteritis?
- Blindness
- Heart failure
- Renal failure
- Lung fibrosis
- Stroke
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |