Playlist
Show Playlist
Hide Playlist
Upper Respiratory Infections: Diagnosis and Management
-
Slides UpperRespiratorySymptoms AcuteCare.pdf
-
Download Lecture Overview
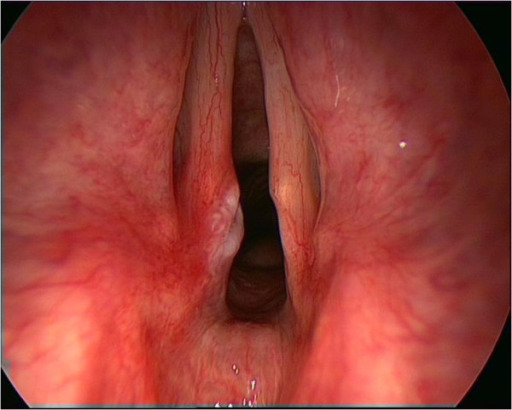
00:01 So, let’s return to our coughing man. 00:04 So, we've added to his history now. 00:05 He's got non-productive cough. 00:07 It’s slightly worse at night. 00:08 He has sore throat and malaise. 00:13 In addition, he's had no shortness of breath, no facial pressure. 00:19 He took care of a grandchild two weeks ago and she had an upper respiratory infection. 00:23 He has a history of gastroesophageal reflux disease and seasonal allergies. 00:29 So, let's take a second just to breakdown that history before going to the question. 00:33 So, no fever, no shortness of breath, no facial pressure. 00:37 So, makes it sound like an asthma or COPD exacerbation. 00:41 It is less likely. 00:43 So is sinusitis. 00:44 He's got the target there, the vector case of his grandchild probably gave him the URI that history matches up really well. 00:51 He also has a couple of reasons for chronic cough in there as well, with the GERD and the seasonal allergies. 00:56 So, that’s something to consider. 00:58 So, putting that altogether, though, what do you think is the most likely source of this patient's symptoms? Is it, A typical bacteria such as a pneumococcus; B, a typical bacteria such as mycoplasma; C, GERD and the allergic rhinitis, just exacerbation of those together; or D, viral infection? And the answer is D. 01:18 This came on more abruptly. 01:20 It’s a one-week history. 01:22 The cough, worse at night, probably consistent with a little post-nasal drainage. 01:27 He has sore throat and malaise, which you wouldn’t necessarily get with a GERD and allergic rhinitis, and he has the upper respiratory infection contact. 01:34 So, it sounds very much like a typical cold. 01:39 So, of course, you’re going to do physical on this patient. 01:42 Things that I look for, his nares might tell you a little bit of a story, maybe more erythema in a patient with an infection, maybe more blue or boggy mucosa in somebody with rhinitis alone, allergic rhinitis in particular. 01:56 In the oropharynx, watching out for pharyngitis. 01:59 So that differences – are there exudates or no exudates. 02:02 Erythema is going to be very common because of all the drainage that patients have down their throat. 02:08 Lymphadenopathy would also suggest an acute infection versus just something related to his GERD and rhinitis. 02:14 And of course, listening to the lungs. 02:16 If there's any lung finding, it's almost certainly going to make me consider a chest x-ray, particularly if it’s a new finding because I'm worried about pneumonia. 02:27 The most common finding, classic being rhonchi, but you can hear crackles and sometimes wheezes too. 02:31 Whereas in the typical viral upper respiratory infection, lungs are clear. 02:38 I think one of the most difficult things is trying to differentiate clinically influenza versus common cold. 02:44 It's important clinically because you want to institute treatment for influenza as fast as possible, at least within 72 hours of symptom onset for the antiviral drugs to be effective. 02:55 One simple way to break it down is more systematic symptoms. 02:59 Think of influenza. 03:00 More localized symptoms to the head and to the throat, think of a common cold. 03:06 So, influenza, it’s just going to – it’s going to knock you out. 03:09 You’re going to get more myalgia, more fever, more headache, more fatigue, more of those constitutional symptoms across your entire body. 03:17 And you also get a more severe cough. 03:20 Whereas a common cold, you’ll get more sore throat, more sneezing, more nasal congestion. 03:25 So, localized symptoms to the upper respiratory tract alone. 03:30 It’s a help, but it’s still – physicians are pretty bad at predicting clinically what's influenza versus a common cold, particularly at the incipient stages of illness. 03:41 So, back to the coughing man. 03:43 His exam reveals some erythema of his turbinates. 03:46 He’s got posterior – he’s got erythema in his posterior oropharynx as well, but no exudates, and he has some posterior cervical lymphadenopathy and clear lungs as well. 03:56 So, given that, let’s think about treatment because I think diagnosis of upper respiratory infection is cinched in my mind now, let’s think about how we can make him feel better. 04:07 So, is the best idea strict bed rest for a few days? Can analgesics help his malaise? Or C, Amoxicillin or macrolide will reduce the duration of his symptoms? Or D, decongestants have the best record of efficacy in improving your eye symptoms? The answer is B. 04:23 So, let's talk about the care for the common cold. 04:27 Maybe dispel some myths along the way. 04:29 First of all, antipyretics/analgesics should be a mainstay of therapy because they are very safe and generally very effective, particularly when taken for the short term. 04:37 For children, for particularly upper respiratory symptoms in terms of the cough and congestion, there is no medicine unfortunately that's really been found to be consistently effective. 04:48 And yet, many parents will employ antihistamines and employ cough suppressants. 04:54 That often can lead to grogginess and rarely can lead to more symptoms among children. 04:59 So, therefore, really try to avoid those if possible. 05:03 But I can tell you, again from personal experience, that nasal suction really works and there's products which you can create, using your mouth as suction, negative pressure and that works a heck of a lot better than a simple bulb and we’re talking about particularly here for infants. 05:18 As they get a little older, they can blow their own nose, but it's really terrible to see a four-month old struggling with a very stuffy nose. 05:26 And so, there are some commercial products out there, fairly cheap, that really do work well to suck out that snot. 05:33 That said, whoever invents a cure – and you’re all young physicians. 05:36 If you invent a cure for pediatric snot, you should absolutely win a Nobel Prize. 05:41 And call me because I’ll personally send you money because it's really necessary and important in this planet. 05:47 For adults, guaifenesin has some mixed record of evidence. 05:52 Some studies say it works; some studies say it doesn’t. 05:55 Mucolytics generally may improve symptoms. 05:58 They’re fairly side effect free. 06:00 So, certainly consider them, particularly for patients who have a lot of congestion. 06:04 Bed rest is good for keeping the infection localized, but it isn’t really going to make a difference in the duration of illness. 06:11 It may feel better, but patients who continue to go to work get better at about the same rate regardless. 06:17 And then, certainly, I want to practice good stewardship, and that means avoiding the broad use of antibiotics for most cases of upper respiratory infection. 06:26 Let’s talk about antibiotic use. 06:29 So, when antibiotics may be necessary? So, one of the cases is rhinosinusitis. 06:33 Our case did not have it. 06:34 He didn’t sinus pressure. 06:35 He didn’t have a long duration of symptoms. 06:37 Duration doesn't correlate perfectly with the risk of sinusitis, but generally it's accepted that symptoms that are persisting for more than 10 days or getting worse, that means it might be time – and particularly when they’re associated with facial pressure and continued congestion, that's when rhinosinusitis may be in order. 06:56 Don't use the broad-spectrum agents. 06:59 You can stick to specific and simple antibiotics, such as amoxicillin. 07:04 Works just as well. 07:06 And it’s going to be – promote less antimicrobial resistance. 07:10 The treatment period is considerable, and that's something that patients need to commit to. 07:15 They might feel better sooner, but definitely have them take the antibiotics for at least 5-7 days once they commit to them. 07:22 For the other considerations, the patient who doesn't usually have cough, doesn't have a lot of congestion, but does have pharyngitis with lymphadenopathy and also has some exudates on the throat, that patient probably has a group A streptococcal infection. 07:36 Penicillin still preferred. 07:37 It’s a 10-day course. 07:39 It doesn't really improve the duration of symptoms that much. 07:43 Maybe by a day or two. 07:44 But it does prevent rheumatic fever, and that's why penicillin is recommended n cases of group A streptococcal infection. 07:50 It does not, however, improve the risk of post-streptococcal glomerulonephritis. 07:55 These are rare complications of a streptococcal infection, which is a fairly common one, but nonetheless they’re important complications because they can have serious consequences. 08:04 And just remember, as always, a great way to diagnose Epstein-Barr virus that you weren't thinking about is giving the patient amoxicillin for it and they break out in a rash. 08:12 That's very pathognomonic for Epstein-Barr infection. 08:19 And so, hopefully, you have learned some tricks in identifying viral upper respiratory infections and differentiating the type of infection a little bit, particularly the ones that might need antibiotics. 08:30 And we covered some treatments, limited as they may be, for improving symptoms in the common cold. 08:38 I think the key is really be upfront with your patients. 08:41 Practice shared decision-making. 08:43 And do no harm in recommending a whole wide array of over-the-counter products or other treatments for the common cold because they might – they’re probably not going to work and they might produce some serious side effects. 08:55 Thank you.
About the Lecture
The lecture Upper Respiratory Infections: Diagnosis and Management by Charles Vega, MD is from the course Acute Care. It contains the following chapters:
- Diagnosis of Influenza and Common Cold
- Management of Upper Respiratory Infections
Included Quiz Questions
Which of the following is the most appropriate in the management of a 5-year-old child with the common cold and normal sleep and oral intake?
- Medications have no proven benefit for children with the common cold.
- Dextromethorphan
- Diphenhydramine
- Chlorpheniramine maleate
- Nasal pseudoephedrine
Which of the following is most likely the main indication for antibiotic treatment in children with group A Streptococcus pharyngitis?
- Prevention of acute rheumatic fever
- Reducing symptom severity
- Prevention of post-streptococcal glomerulonephritis
- Reducing symptom duration
- Prevention of spread to others
Which of the following symptoms is more suggestive of influenza rather than the common cold?
- Myalgia
- Nasal congestion
- Sore throat
- Sneezing
- All of the listed choices are more suggestive of common cold
A previously healthy 41-year-old woman presents with 2 weeks of nasal congestion, headaches, general malaise and mild fevers. Her symptoms of nasal congestion and cough had initially improved after a few days when she started feeling sick again with worsening nasal congestion, fever and headaches. She denies any shortness of breath. Her vital signs are within the normal limits. On physical examination, she has mild tenderness over the frontal sinuses. She has mild nasal congestion and postnasal drip. The remainder of the physical examination is unremarkable. Which of the following is the most likely diagnosis?
- Rhinosinusitis
- Influenzae
- Atypical pneumonia
- Allergic rhinitis
- Common cold
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This everyday clinical cases may be the most important lesson for new doctors.