Playlist
Show Playlist
Hide Playlist
Postoperative Care (Part 2)
-
Slides Post-operative care Special Surgery.pdf
-
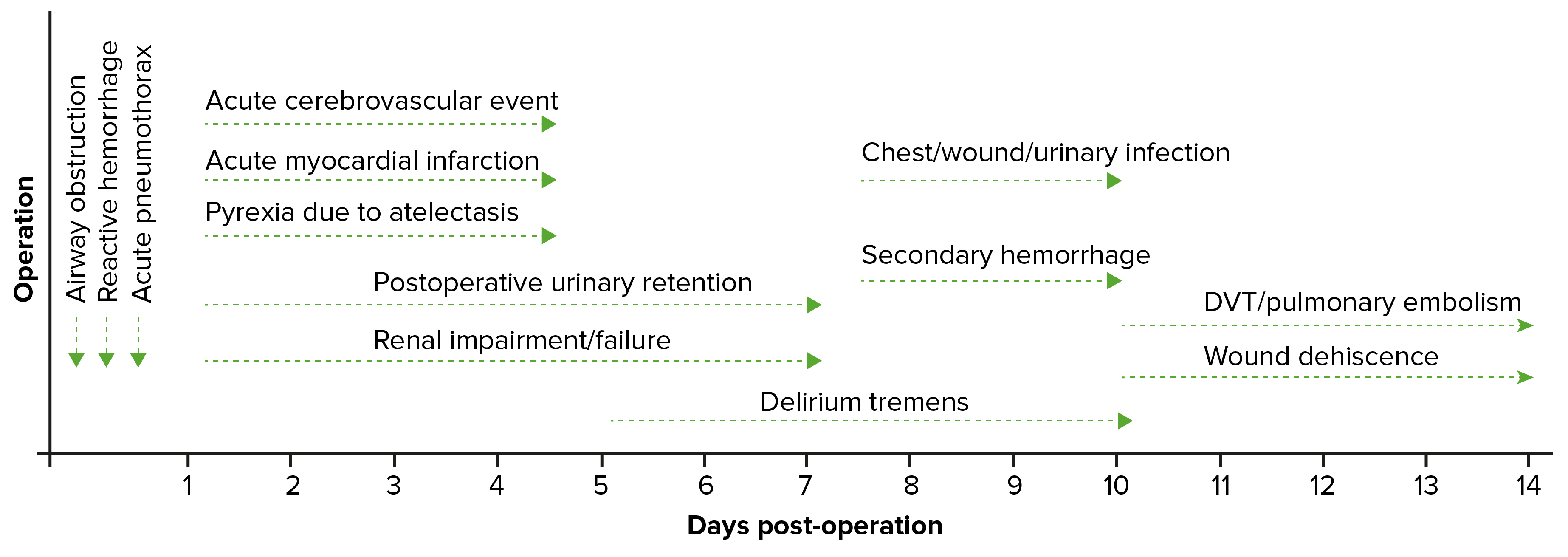
Download Lecture Overview
00:01 Let's ask you a question about a clinical scenario. 00:05 A ward nurse calls you in the post-op period to report desaturation in your patient. 00:10 What might be some of the causes of a low saturation or a pulse oximetry. 00:15 I'll give you a second to think about this. 00:20 Here are some etiologies of hypoxia. 00:23 Poor inspiratory effort. 00:25 Sounds silly. 00:26 Patients who have pain splint and do not breathe and subsequently contribute to atelectasis. 00:32 Remember, we do not spend the vast majority of the waking hours in a recumbent position. 00:37 If your patient is immediately postoperative, that's why we encourage them to move about and ambulate. 00:43 We do not want them to be recumbent. 00:45 Recumbency of even a few minutes causes dependent atelectasis. 00:50 As a result of atelectasis, pneumonia can occur. 00:54 A pneumonia in the postoperative period is usually unlikely unless there was already a pre-existing community-acquired pneumonia that was subclinical and not diagnosed. 01:04 And lastly, a very important etiology of hypoxia is pulmonary embolism. 01:10 Pulmonary embolism is a low probability, however, highly significant finding. 01:17 Therefore, we recommend that you have a low threshold for seeking pulmonary embolism, particularly in the postoperative period. 01:27 How do we treat desaturations? First, prior to even knowing exact diagnoses, give the patient supplemental oxygen. 01:34 What if the patient is hypoxic because they’re having a myocardial infarction. 01:37 We want to make sure that enough oxygen is delivered to the systemic system, especially the coronary systems. 01:45 Get an ABG (arterial blood gas). 01:47 Maybe the information can be helpful in terms of diagnoses of pulmonary embolism. 01:52 That is defined by hypoxia and hypocarbio (or low CO2). 01:58 And sometimes, chest x-rays are incredibly helpful, particularly if there's concern for a pneumonia. 02:04 If the clinical scenario warrants or fits, maybe there's a tension pneumothorax or pneumothorax from your procedure. 02:12 Let's move on to a different scenario. 02:14 Now, you’re on call and a different nurse calls and says Mrs. Jones is difficult to arouse. 02:20 What are you thinking? What's your differential diagnosis, particularly in the postoperative period? I'll give you a moment to think about this. 02:31 Mental status changes are common in the hospital, particularly in the elderly. 02:35 Here are some important questions I ask whenever I receive that call. 02:39 First, is the patient protecting her airway? Remember, from our trauma lectures, that an intact airway or a conduit doesn't necessarily mean that the patient is actually moving air. 02:51 That's the BO breathing. 02:53 Remember, if the patient has an inability to protect airway or is not moving air, early intubation is recommended. 03:02 Were their neurological findings consistent with a stroke? These are typically called lateral lysing signs. 03:09 It's fairly rare to have only mental status changes associated with the stroke. 03:13 Typically speaking, there is some one-sided paresis. 03:17 And it’s also important to dig through the chart and make sure that neurological findings were not already pre-existing. 03:25 Lastly, was there a recent sedative or anxiolytic medications administered, particularly in narcotic naïve patients, small doses of morphine or fentanyl can cause significant mental status changes. 03:38 And in the elderly patient, remember, sundowning is very common. 03:43 When we are taken out of our familiar circumstances and surroundings, brought into the hospital and subjected to surgery, one shouldn’t be surprised, particularly in the elderly patient population, that some people get confused. 03:58 Are there any adjunctive studies that we should get? Well, we talked about an ABG, maybe hypoxia is the reason why the patient has mental status changes. 04:07 An EKG. 04:08 An EKG may tell us whether or not the patient has had an myocardial infarction. 04:12 Chest x-ray may explain why there may be a hypoxia or maybe there is an infection that's causing the patient to have mental status changes. 04:20 And, of course, a CAT scan of the head to evaluate for either space occupying issue or a stroke. 04:26 Remember, early on a stroke, the CT head may be completely negative. 04:31 And that might call for a repeat head CT. 04:34 It's fairly unlikely for a patient to have new onset bleed unless they fell in the hospital. 04:40 Using DVT chemical prophylaxis alone has very, very low incidence of intra-hospital intracranial bleeding. 04:48 Now, let's go over some important take-home clinical pearls and high-yield information. 04:53 Remember, sometimes in the postoperative period, you might have to institute therapy prior to knowing the diagnosis. 05:00 For example, Mrs. Jones who had altered mental status, although you may not know why she has altered mental status if she's not having a protected airway or breathing, you will have to intubate the patient prior to having the actual diagnosis. 05:15 After you manage the life-threatening deterioration, you then move on to further workup. 05:23 High-yield information for your examination. 05:26 Please consider pulmonary embolism in a patient who is hypoxic and hyperventilating. 05:32 Hyperventilation is demonstrated on an arterial blood gas (or ABG) as low carbon dioxide. 05:39 Thank you very much for joining me on this discussion of postoperative care.
About the Lecture
The lecture Postoperative Care (Part 2) by Kevin Pei, MD is from the course Special Surgery.
Included Quiz Questions
A nurse pages you that one of your post-operative patients is difficult to arouse. What is your first step in evaluating the patient?
- Make sure the patient is protecting their airway and moving air
- Obtain an EKG
- Check what medications were recently administered
- Check for neurological findings consistent with stroke
- Obtain an ABG
An ABG of a patient shows low carbon dioxide levels. The patient is hypoxic and hyperventilating. Which of the following conditions is your MOST likely diagnosis?
- Pulmonary embolism
- Myocardial infarction
- Air embolism
- Stroke
- Deep vein thrombosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |