Playlist
Show Playlist
Hide Playlist
Pleural Disease: Introduction
-
Slides 09 PleuralDiseases RespiratoryAdvanced.pdf
-
Download Lecture Overview
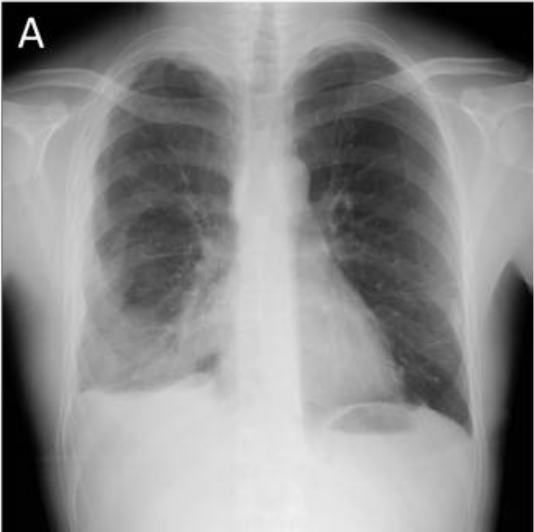
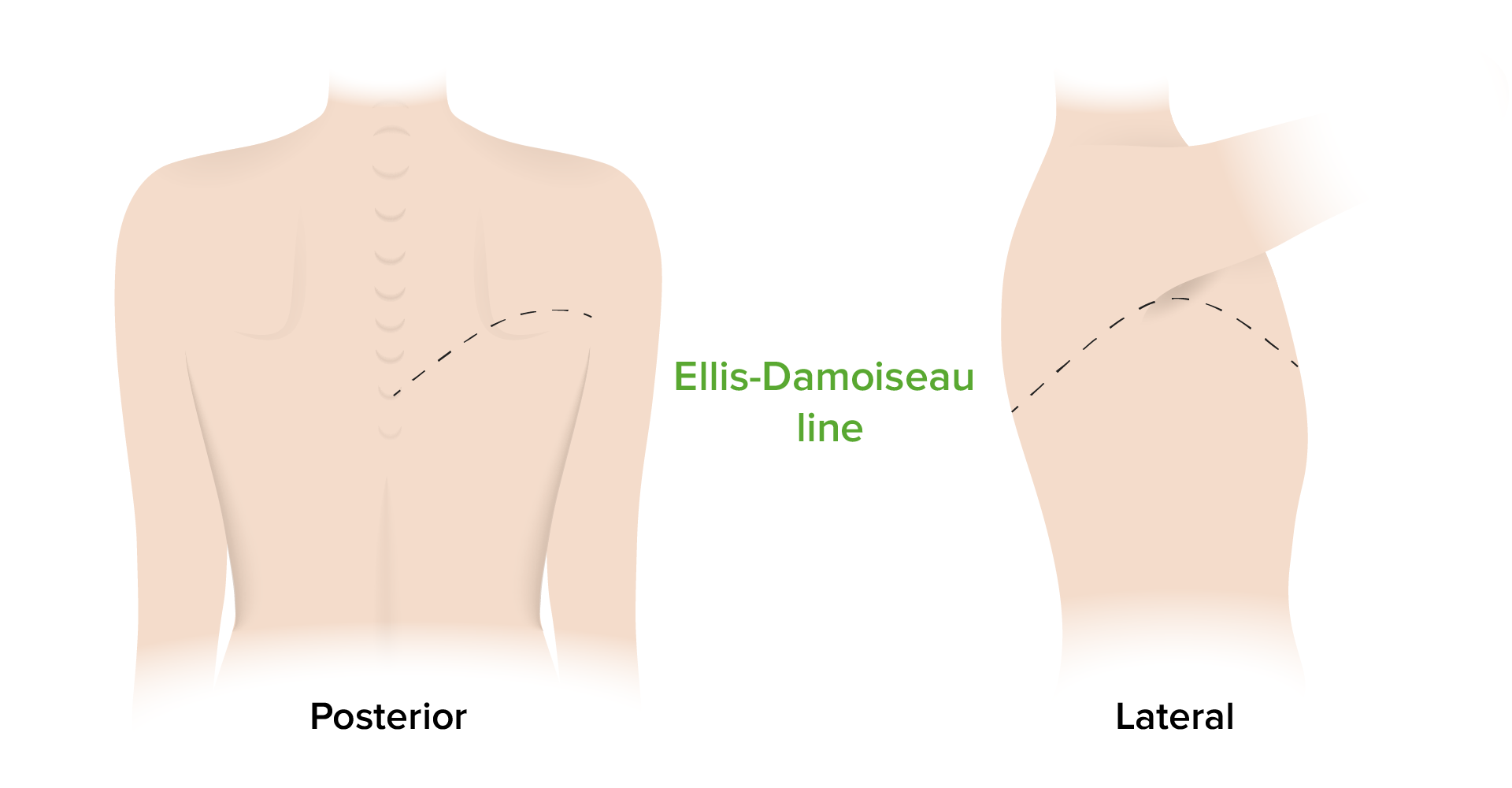
00:01 The subject of this lecture is pleural disease, by which we mean pleural effusions which can be transudates or exudates or infective in origin. In addition, we’ll talk about pneumothorax which is air in the pleural space and pleural thickening. Mesothelioma which is a primary cancer of the pleura is actually discussed in the lung oncology lecture. There are a couple of important basic concepts about pleural disease. The first is that there are no divisions in the normal pleural space. That means that when you have a pneumothorax with air in the pleural space, it will rise to the top, whereas if you have pleural fluid, then it will sink to the bottom and pleural effusions are best detected at the base of the lungs. 00:40 However, if you get an infection in the pleural space or a hemothorax that is blood in the pleural space or a surgeon has done some pleural surgery, then you get adhesions forming between the visceral and the parietal pleura. And that can cause loculations of the pleural space divisions, and that will make the X-ray appearances of pleural fluid or pneumothorax quite different. The other basic concept of pleural space is under negative pressure, and this keeps the lungs inflated. That means that when you get a pneumothorax, the lung will collapse. Pleural disease is actually readily detectable normally by clinical examination. The stethoscope will quite easily pick up a difference when somebody has a pneumothorax or pleural effusion between the affected side and the normal side. 01:29 And percussion will readily pick up somebody with a large pleural effusion. The best test is actually a pleural ultrasound, and that is the most efficient way of assessing for pleural fluid and for divisions in the pleural space and is also affected by identifying whether there are any masses or abnormality of the pleural surface itself. 01:52 So pleural effusions, fluid in the pleural space. This is an X-ray, on the right hand side, of somebody with a left pleural effusion that should be readily detectable clinically. 01:59 And you can see it quite easy on the chest X-ray. These are very common and they occur in multiple different specialties because if the causes are very large range, it will be seen by multiple different medical specialties. The presentation is either as an asymptomatic finding on a chest X-ray or as the effusion gets bigger, the patient becomes more and more breathless. So that causes progressive dyspnoea over days or weeks. 02:25 Sometimes with the more inflammatory types of pleural fluid, those which are caused by infection or perhaps a pulmonary embolus, then pleuritic chest pain is actually a very prominent symptom. Pleuritic chest pain is very specific and very easily characterized. 02:39 It’s a pain that occurs on inspiration and is localized to where the inflammation is occurring normally on one side of the chest. And you may hear a pleural rub over that area. 02:52 So when you examine somebody with a pleural fluid, what you will find is that the trachea of large effusions may be deviated away from the affected side. The expansion of the lung with a pleural fluid around it will be reduced. And when you percuss, it will be very dull over the pleural fluid because the air has been replaced by liquid, and that’s described as stony dull because it’s very dull indeed. You won’t be hearing any breath sounds, and vocal resonance will also be reduced over the area of the effusion. Sometimes at the top of the effusion, you may hear an area or patch of bronchial breathing, and, of course, you may hear a pleural rub that is inflammation of the pleura. But that will be heard with the visceral, and the parietal pleura are actually allowed to pose each other. Therefore, it won’t be heard of the areas of large effusions but areas where the effusion are much smaller. There may be also signs of what the cause of pleural effusion is. So for example, there may be palpable lymph node, somebody has got a cancer or an enlarged liver, if somebody has a cancer with liver metastases, there might be signs of chronic liver disease, heart failure, or rheumatoid arthritis. All of which are associated with pleural effusions in some patients.
About the Lecture
The lecture Pleural Disease: Introduction by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Pleural Disease.
Included Quiz Questions
Which finding is typically found on percussion over the area of the chest with massive pleural effusion?
- Stony, dull percussion
- Hyperresonant percussion
- Resonant percussion
- Dull percussion
- Normal percussion
Which of the following statements is FALSE?
- Normal pleural space has divisions due to connections between the visceral and parietal pleura.
- A small pneumothorax is best detected at the top of the chest.
- A small pleural effusion is best detected at the bottom of the chest.
- Significant pleural disease is commonly detected during a good physical examination of the chest.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |