Playlist
Show Playlist
Hide Playlist
Juvenile Idiopathic Arthritis (JIA): Diagnosis & Management
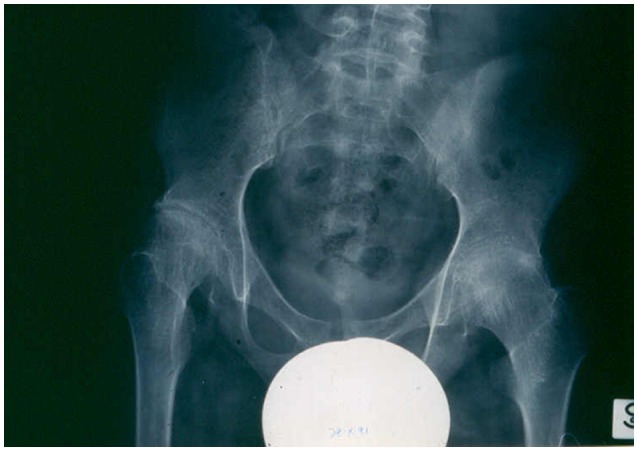
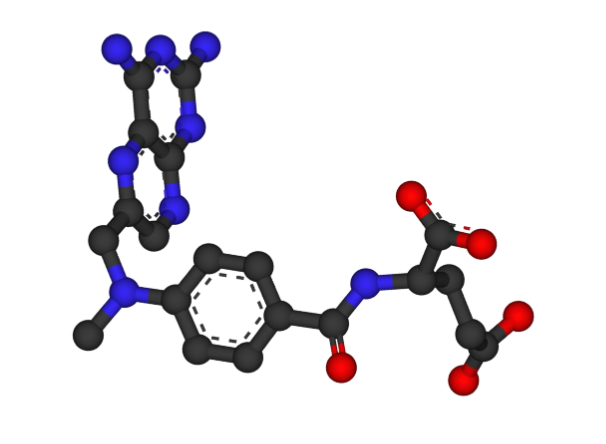
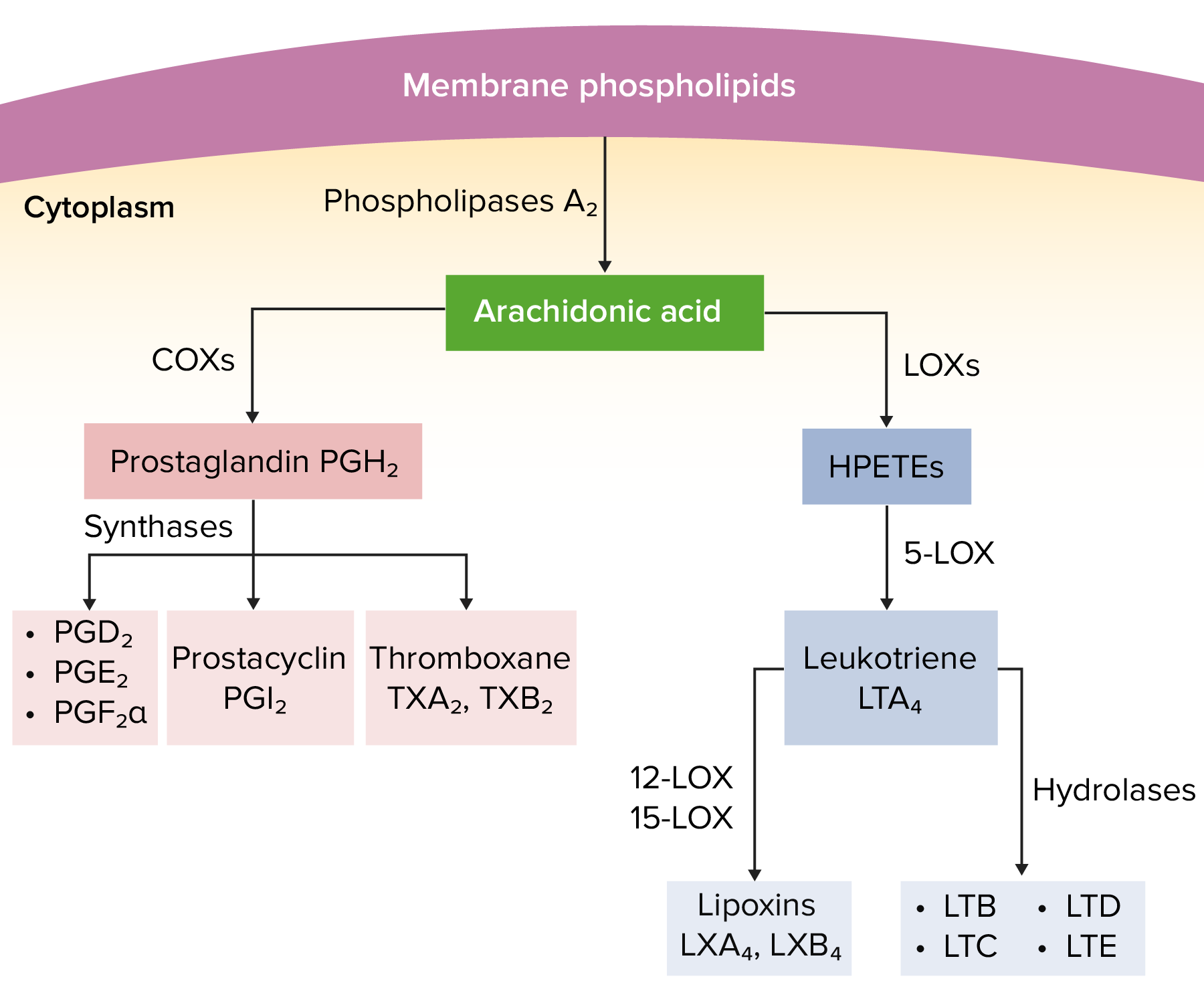
00:01 There are some labs which you may need to help you identify JIA but there’s no one lab that is totally diagnostic. We will often see in these patients very elevated erythrocyte sedimentation rates. 00:14 An ESR of 140 would not be atypical. But if the patient has an ESR that’s elevated but say only, I don't know, 30, it’s seems very unlikely that patient will have JIA. Additionally, the CRP may be elevated. 00:28 The patient may have a high white count, sort of like a stress response and likewise high platelets, again an inflammatory stress response. People hear JIA and they think JRA which was our old name for this disease. We used to call it juvenile rheumatoid arthritis. One of the reasons that we stopped using this is the rheumatoid factor is actually a bad screening test for this disease. Keep in mind, most kids with the disease do not have a positive rheumatoid factor. The rheumatoid factor if positive predicts chronic erosive joints in those patients with polyarticular JIA. So, it may be useful prognostically or therapeutically in deciding what variety of polyarticular JIA is going on. But it's not a good screening test if you’re asking yourself is this child with some swollen joints having JIA? The ANA is also obtained. 01:29 It is associated with an increased risk of involvement of the eye specifically uveitis. Certainly, in a patient with JIA who has a positive ANA, I would refer that patient to an ophthalmologist for an evaluation. 01:43 The HLA-B27 type is increasing risk for enthesitis in patients with enthesitis-associated JIA. 01:54 So, that would be a marker for enthesitis-associated JIA but HLA typing is not commonly done in these patients. 02:03 If we were to image a joint, let’s say we thought maybe it was an infected joint or something like that, what we’ll see in that joint especially on MRI is erosive changes and inflammation. You can certainly see it on X-ray too as a later finding. Here, we have an MRI of a child with JIA. You can see that knee is really taking a beating. There are areas of degradation and erosion in the knee joint that are going to cause this child problems. The management of JIA is mostly around restricting inflammation in these patients. The first line of therapy is NSAIDS. We will use usually long-acting NSAIDS like naproxen to control the swelling and control the pain. If naproxen isn’t doing the trick, we may do joint injections or rarely systemic steroids in a particularly bad inflammatory period. 03:00 Injected steroids are a good temporizing measure for any joint that’s having significant inflammatory process. Lastly, if joint injections and NSAIDS aren’t doing the trick, we may put these children on systemic significant anti-inflammatories like methotrexate. Remember, if a patient is on methotrexate, you need to follow their CBC and their LFTs every few months to watch for neutropenia and transaminitis. 03:29 The indications for biologic agents are complicated, and this is not information you need to memorize. 03:34 But understand that a wide variety of biologic agents designed at inhibiting specific parts of the immune system are used in an off-label way in these children to help control inflammation. 03:47 Treating complications of JIA is important. Patients can get all kinds of problems as a result of living with this autoinflammation. One possibility is they can grow poorly and in particular, they can have leg length discrepancy. Doctors can refer patients for special shoes where one shoe has a lift to accommodate leg length discrepancy. We don’t want children to be chronically walking with the hip out of kilter. For uveitis, we are going to have patients follow frequently with ophthalmologists who are going to help us manage these patients especially if they’re ANA positive. Occasionally, especially in enthesitis and other severe joint involvement, patients could get contractures. This requires physical therapy, botox injections, and muscle relaxants most like we manage cerebral palsy. For patients with growth problems in general, we want to watch their growth carefully. Not only can their growth happen as a result of bony problems but in an autoinflammatory and very inflamed state, kids sometimes just don’t grow particularly well. 04:54 In terms of prognosis, oligoarticular JIA probably has the best prognosis and oftentimes, these children will achieve a state of remission. Rheumatoid factor positive oligoarticular JIA has the lowest likelihood of remission and can persist into adulthood as other varieties of arthritis. 05:17 The prognosis for systemic JIA depends on the extent of the arthritis and the systemic symptoms after six months of therapy. Some children get all the way better and get better and they’re fine. 05:28 Other children can progress to other stages or types of arthritis and problems later on in life. 05:37 That’s all I have to tell you today about juvenile idiopathic arthritis. Thanks for your time.
About the Lecture
The lecture Juvenile Idiopathic Arthritis (JIA): Diagnosis & Management by Brian Alverson, MD is from the course Pediatric Rheumatology and Orthopedics. It contains the following chapters:
- Diagnosis of JIA
- Management of JIA
Included Quiz Questions
Regarding juvenile idiopathic arthritis, which of the following statements is TRUE about the rheumatoid factor? Mark all that apply
- It is a bad screening test for JIA.
- A positive test is associated with the risk of uveitis.
- It is usually positive in enthesitis-associated JIA.
- It is usually positive in systemic JIA.
- A positive test predicts chronic erosive joints in polyarticular JIA.
Regarding juvenile idiopathic arthritis, which of the following clinical problems does NOT match the proposed management?
- Uveitis - antibiotics
- Joint inflammation - steroid injections
- Contracture - botox injections
- Growth problems - careful monitoring
- Leg length discrepancy - special shoes
Which of the following statements regarding the prognosis of a patient with juvenile idiopathic arthritis (JIA) is TRUE?
- Oligoarticular JIA has the highest rate of remission.
- RF-positive oligoarticular JIA has the highest likelihood of remission.
- Oligoarticular JIA does not progress into adulthood.
- The prognosis of systemic JIA depends solely on the age of the patient.
- ANA negative patients have a greater risk of uveitis.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture. Very well-explained, clear and concise, informative. Thanks!