Playlist
Show Playlist
Hide Playlist
Nephritic Syndrome
-
Slides NephriticSyndrome IgA Nephropathy RenalPathology.pdf
-
Download Lecture Overview
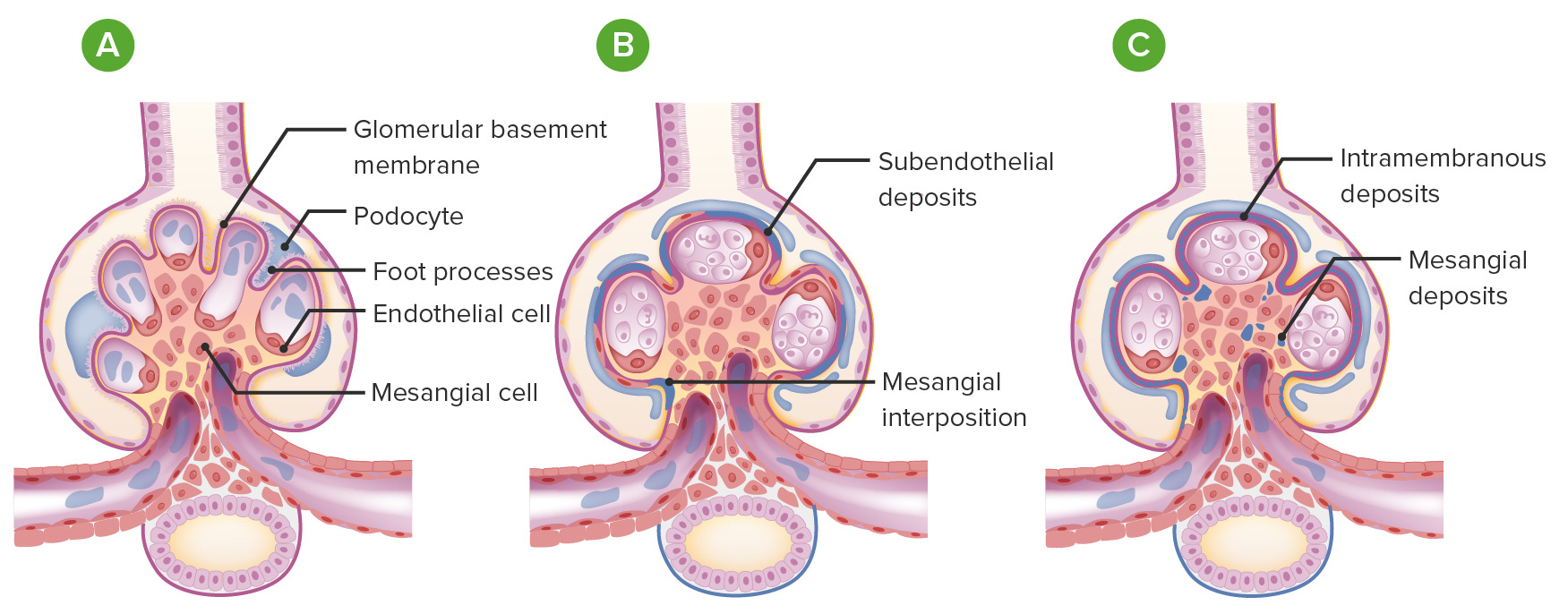
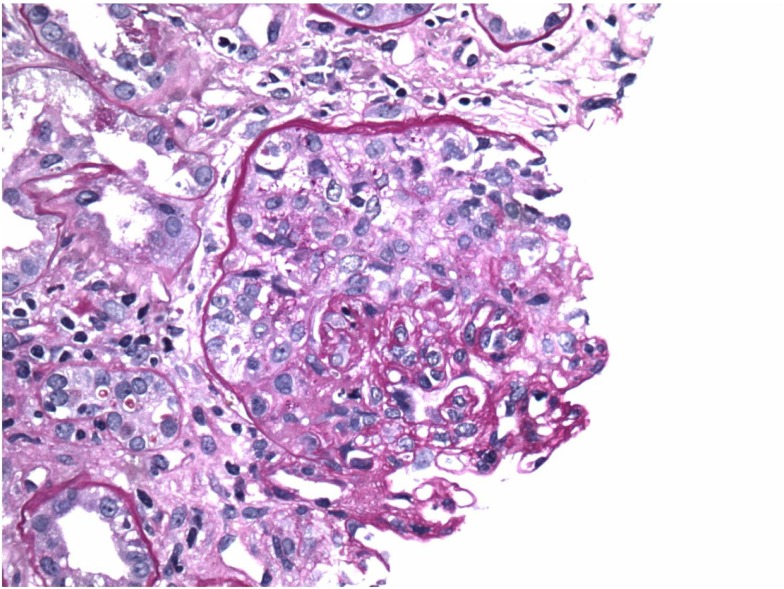
00:01 With nephritic, the primary disorder is dealing with neutrophils. 00:05 Keep that in mind. 00:06 Because I've asked you to focus on that H, let’s take a look at hypertension. 00:10 Now, understand, whenever there is issues of renal failure or issues with the kidney in general, you are going to retain that sodium therefore contributing to that hypertension. 00:20 Now, when I say there is massive protein loss with nephrotic syndrome, understand that even nephritic, you are going to lose protein but it will not be as much as 3.5 grams of protein loss per day. 00:36 Greater than 3.5 grams of protein loss per day automatically puts you in the category of nephrotic and it’s edema in nephrotic will be significant. 00:48 You are still going to loss protein with nephritic syndrome, but not as greatly. 00:54 So therefore here, the type of edema will be peri-orbital type of puffiness and once again, usually due to that salt retention and resulting in increase hydrostatic pressure. 01:07 Edema can be more generalized however, remember, the type of edema is not going to be as profound as what you find with nephrotic. 01:17 Next, along with hypertension and mild edema, peri-orbital puffiness, the fact that you are producing very little urine, oligo. 01:28 Last time that we looked at the term prefix oligo was when we're dealing with hydramnios, little amniotic fluid. 01:36 This is little urine production, oliguria. 01:40 We have approximately, and you must know the definition, of approximately 400 ml of urine being produced per day. 01:48 Day, you pay attention to units. 01:50 Due to once again, decrease GFR from an inflamed glomeruli, hence the neutrophils coming in. 01:59 Here’s your second H, the hematuria. 02:01 Now, with the hematuria, what does that mean? What type of RBC have we discussed earlier that would then lead you to think that the damage will actually took place with the glomerulus? And that in fact would be a dysmorphic RBC. 02:15 What does that mean? As an RBC passes through the glomerulus, there’s every possibility that there might be a part of that biconcave RBC which might not be an out-pouching. 02:28 That’s a dysmorphic RBC. 02:30 Irregular membrane due to inflamed glomeruli from immune-complex deposition. 02:37 Let me give you a prototype for nephritic syndrome and actually, let me give you two of them. 02:41 One was called IgA nephropathy, aka, Berger, and the other one would be post-streptoccocal glomerulonephritis. 02:48 And as the RBC’s trying to make it through it might then become dysmorphic. 02:53 Now, your laboratory findings are irrelevant for nephritic include the fact that you would find neutrophils in the sediment. 03:00 Particularly in the immune complex type so that’s more involved with inflammatory processes. 03:07 The RBC casts are key findings. Now, let me walk you through this real quick with nephritic. 03:12 Number one. H, hypertension, under hematuria, we have RBC casts and we have dysmorphic RBCs. 03:21 Do you see as to how that fits in perfectly? We just need to make sure that you organize your patterns and thoughts accordingly. 03:29 The proteinuria will be less than 3.5 grams per day. 03:33 That’s important that you pay attention to. 03:35 Yes, greater than 150 mg, but definitely less than 3.5 grams per day, because anything beyond this, what category does that put you in? Very good, nephrotic. 03:48 Under nephritic, your BUN/Creatinine ratio, well, tubular function is intact in acute glomerulonephritis. 03:56 And that’s very important for you to understand. Why? Give me a condition in which your tubules are also damaged. 04:06 Good. That’s called acute tubular necrosis, isn't it? So when you have acute tubular necrosis, the physiology behind that is the fact that you cannot reabsorb any, any urea. 04:20 Where is urea in this ratio? B, blood, U, urea, N, nitrogen. 04:27 Ah, there’s urea. 04:29 So in acute tubular necrosis, you can expect that ratio to be decreased. 04:33 However, in acute glomerulonephritis, you can still expect your azotemia to be relatively elevated. 04:40 Isn’t that interesting?
About the Lecture
The lecture Nephritic Syndrome by Carlo Raj, MD is from the course Glomerulonephritis.
Included Quiz Questions
Which of the following laboratory findings is used to differentiate nephritic syndrome from nephrotic syndrome?
- Proteinuria < 3500 mg/day
- BUN:Cr ratio > 15
- BUN:Cr ratio < 15
- Proteinuria > 150 mg/day
- Proteinuria > 3500 mg/day
Which of the following causes the primary damage to the glomeruli in nephritic syndrome?
- Neutrophils
- Lymphocytes
- Eosinophils
- Monocytes
- Basophils
Salt retention leads to which of the following clinical manifestations in nephritic syndrome?
- Hypertension and periorbital puffiness
- Hypotension and periorbital puffiness
- Hypertension and pretibial puffiness
- Hematuria and perioral puffiness
- Hyperproteinemia and periorbital puffiness
What is the definition of oliguria?
- Less than or equal to 400 mL of urine in 24 hours
- Approximately 400 mL of urine in 12 hours
- Approximately 1000 mL of urine in 48 hours
- Approximately 40 mL of urine in 24 hours
- Approximately 4000 mL of urine in 24 hours
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |