Playlist
Show Playlist
Hide Playlist
Asthma: Subtypes and Diagnosis
-
Slides 03 Asthma RespiratoryAdvanced.pdf
-
Download Lecture Overview
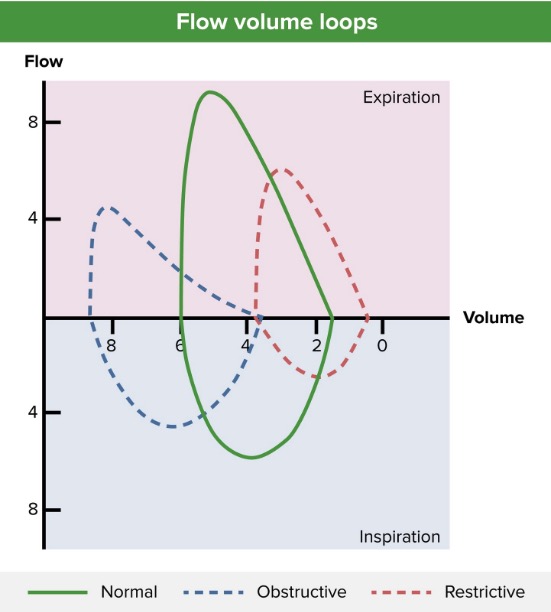
00:00 worse asthma. And this is a major driver for many patients conditions. So, we can characterize asthma into various different subtypes as well. Chronic asthma, this is when you’ve developed an element of irreversible disease leading to chronic dyspnoea or a chronically low FEV1, and reflects poorly controlled disease over many years. 00:18 An exacerbation, that’s an acute deterioration stimulated often by the triggers we’ve just discussed. A severe asthma is an attack of asthma that’s bad enough to require admission to hospitals. So as in exacerbation, they require somebody to come into the hospital. 00:34 Status asthmaticus is one level above that where you have an exacerbation which is severe enough to be life-threatening and requires very close attention to treatment to ensure that the patient gets better. And there is not an instant response. It’s not with a less severe exacerbation. One dose of nebulizer is probably normal enough to restore them to reasonable health. In the status asthmaticus, it requires much more intense treatment there. Doctors often use the phrase bronchospasm, and all they mean by that is an episode of increased bronchial obstruction or an increased episode of airways obstruction, and that essentially is an exacerbation. Other subtypes of asthma include brittle asthma. 01:20 These are patients who actually are relatively well most of the time but then can have sudden exacerbations which can be very rapidly developing. I have a patient who went down into the kitchen one day feeling perfectly well, and next time she woke up, she was in hospital intensive care. And what had happened is that somewhere in the kitchen, something had set off her asthma attack. And fortunately, the postman found her when he came to deliver a parcel that day. Otherwise she would have been dead. That’s brittle asthma, very rapid attacks, rapid falls in peak flow, very severe, and because of that, very dangerous disease. Difficult asthma is a range of problems. It’s when the asthma is poorly controlled and causing major symptoms for the patient or frequent admissions to hospital. It’s defined as difficult asthma when it’s poorly controlled despite extensive treatment and there are a variety of reasons why that might be not responding to the treatment. 02:14 Steroid-resistant asthma is a subtype of difficult asthma which is very specific. It’s where steroids which normally work very well in asthma are not working. The type of information that patient’s asthma is due to does not respond to corticosteroid therapy for whatever reason. Cough-variant asthma is essentially very mild asthma where the only symptom the patient has is cough, and this one is quite hard to diagnose because there’s no wheeze and breathlessness and patients don’t think that the cough could be due to asthma and nor to their doctors either. Occupational asthma, we’ve already discussed, that’s asthma that’s settled by inhaled allergens that you come across during your occupation. It’s very important to identify because clearly, the patients would need to change their job circumstances, either change their job or make sure they have protective equipment when they’re doing their job to try and minimize the disease problems. 03:08 So, how do you make a diagnosis of asthma? Essentially, we need to prove the reversible airways obstruction. Now as I mentioned, clinically, that may be obvious in some patients, and therefore, the requirements to prove that it’s present is not so important. But it can be proved in other ways. One is by response to treatment. If somebody comes to you with episodes of cough and breathlessness and wheeze and these sounds very much like they have asthma, perhaps, this diurnal variation is worse in the morning, the cough wakes them at night. Every time they get a cold, it’s made worse. 03:42 Those sorts of patients, you probably don’t actually need to do too much besides give them the right treatment. And if they get better, then that’s asthma. If you really want to prove it’s asthma, peak flow recordings are a good way of doing that. Now, these record the airflow during expiration, and they show diurnal variation in asthmatics. So for example, in this chart you see on the right-hand side of the slide, there's a big fall in the peak flow in the morning. Now, when you start to inhale steroid, what happens is that the peak flow will gradually improve as the asthma comes under control, but not only that is at the difference between the morning and evening, the diurnal variation becomes smaller. 04:24 So the home peak flow recordings, with and without treatment, are a very good way of identifying patients who have asthma for sure. And you can also use spirometry, the FEV1, and I showed that in a spirograph earlier with FEV1 which improves substantially after bronchodilator showing significant reversible disease, and therefore if the patient has asthma. 04:44 Other tests, well, blood tests may show degree of blood circulation eosinophilia. And then the patient often has a raised total IgE and can be allergic to aspergillus, especially if they have allergic bronchopulmonary aspergillosis which is a complication of asthma, which are discussed in a subsequent lecture. The chest X-ray is necessary to make sure you’re not missing any other diseases, but essentially, is normal in most patients of asthma unless they have an acute attack of chronic severe disease. In which case, that will show hyperexpanded lungs. But as I said, a chest X-ray is vital during exacerbations at least to just make sure there’s no other complication such as a lobar collapse or an infection. 05:26 We often do skin prick tests in patients with asthma, and that’s to identify specific allergic triggers for allergic asthma, house dust mites, cat fur, etc. In many ways, it’s not very practical because if a patient knows that a cat will upset his or her asthma, then they avoid cats. It’s only particularly relevant I suppose for patients where you might be considering allergic bronchopulmonary aspergillosis as a diagnosis in which case, the skin prick test will be positive to aspergillosis. Occasionally, you might come across a patient where it’s quite hard to identify they have asthma. And then we might do things like a histamine or methacholine challenge tests where the patient inhales histamine or methacholine and that causes bronchoconstriction in patients who have asthma. But it doesn’t in patients who don’t have asthma. So that’s inducible airways obstruction. It’s quite a tricky test. It needs to be done in the hospital in a fully equipped pulmonary function laboratory But it can be used to identify difficult cases of asthma to diagnose. And the sputum itself may show the evidence of airways information with the presence of eosinophilia when you send the sputum off for cytology. How do you treat asthma? Essentially, it’s
About the Lecture
The lecture Asthma: Subtypes and Diagnosis by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Airway Diseases.
Included Quiz Questions
Which of the following is the definition of status asthmaticus?
- A severe, life-threatening asthma attack that does not rapidly respond to conventional treatment
- An acute deterioration often related to obvious triggers
- Irreversible disease, leading to chronic dyspnea
- An episode of asthma severe enough to require hospital admission
- An episode of increased bronchial obstruction
Which of the following best describes patients with "brittle" asthma?
- Prone to sudden exacerbation with a rapid fall in PEFR
- Poorly controlled asthma despite extensive treatment
- Poor response to steroid therapy
- Cough as the only symptom
- Asthma triggered by an occupational cause
Which of the following cells are usually elevated in the blood of a patient with asthma?
- Eosinophils
- Neutrophils
- Monocytes
- Basophils
- Lymphocytes
Which of the following immunoglobulins is usually elevated in patients with asthma?
- IgE
- IgA
- IgM
- IgG
- IgD
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |