Playlist
Show Playlist
Hide Playlist
Erythema Multiforme and Stevens-Johnson Syndrome (SJS) in Children
-
Slides EMandSJS Pediatrics.pdf
-
Download Lecture Overview
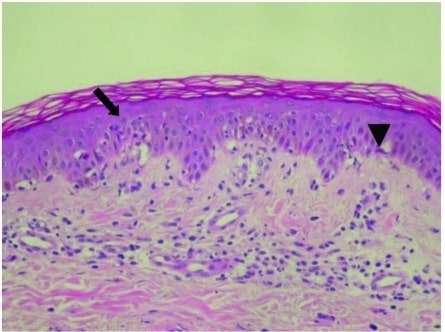
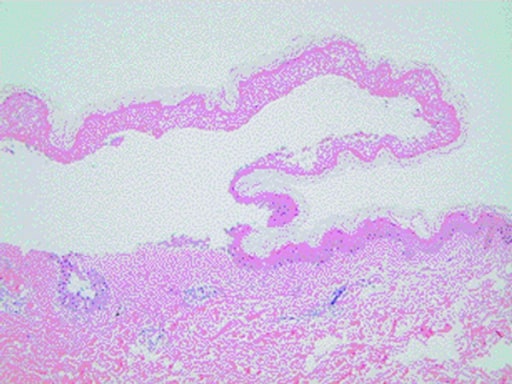
00:00 In this lecture, we're going to talk about Erythema Multiforme and Stevens-Johnson Syndrome. 00:07 So, erythema multiforme is a hypersensitivity reaction. It usually happens to infections such as HSV or mycoplasma or just viral illness. Rarely, it can be a drug reaction or it can be from cancer, collagen vascular disease or it may be idiopathic and people just don't know what's causing it. The lesions may be vesicular or bullous but usually they're targetoid lesions with a central papule surrounded by an erythematous ring usually around 1 to 3 cm. This is a particularly severe case right here, you can see. Generally, they'll have a keratinocyte injury and you can see some necrotic keratinocyte here with a lymphocytic infiltration and on the skin you can see a sort of central area where it's very red on a milder erythematous base. So let's go through the causes of E. multiforme, certainly infections. HSV and mycoplasma are most common but also could be from coccidioidomycosis or histoplasmosis or typhoid or even rarely leprosy. Drugs can also cause this and we usually think of sulfas and penicillins but but there are other drugs such as barbiturates, NSAIDs, or any anti-malarials that can also cause this reaction. Likewise, diseases can cause this such as cancer or lupus or dermatomyositis or polyarteritis nodosa, basically diseases with a lot of antibodies. The treatment for erythema multiforme is largely supportive. It maybe itchy and we give antihistamines but generally this rash is self-limited and will gradually go away on its own, maybe in a week or two. There is a more severe form of this problem, which is Stevens-Johnson syndrome. In Stevens-Johnson syndrome, patients develop severe bullous form of erythema multiforme with widespread mucous membrane involvement and skin involvement and it can be life threatening. It's caused by generally, again, drug sensitivity or infection and it's immune-mediated, often about 1 to 3 weeks after the exposure. The morbidity and mortality in Stevens-Johnson syndrome is generally from dehydration or superficial infection of the sloughed skin. It can also be from toxemia or renal damage and the rate of mortality is low but reasonable, around 1 to 3%. So, let's talk about what this presents like. Patients often have a prodrome of fever, malaise, or URI symptoms. They are prodrome to the illness. Then they develop the rash. This can involve and must involve for diagnosis at least 2 mucous membranes. They can have severe ulceration of the mouth or they can have significant involvement of the conjunctivitis, corneal ulceration, or even uveitis. They may also have genital involvement. Patients generally develop very severe skin disease and they can form bullae which can then slough off and create denuded skin which can be the source of both infection and dehydration. Here's an example of very severe keratinocyte apoptosis and epidermal detachment, so you can see the epidermis can just lift right off. So, to make the diagnosis we generally want to see the typical lesions of targetoid or atypical skin lesions and involvement of at least 2 mucous membranes. One sign of Stevens-Johnson syndrome that might show up is Nikolsky's sign. Nikolsky's sign is when you press down in 1 area adjacent to a bullae and it actually lifts the skin away in the affected area. So this is a sort of like press next to it and the skin sloughs off. That's classic for Stevens-Johnson syndrome. When we're worried about patients, we want to calculate the percent of epidermal detachment. This is treated similarly to burns. If a patient has less than 10% of body surface area involved, we call that Stevens-Johnson syndrome. If it's more than 30%, it is life threatening and we call that toxic epidermal necrolysis. So how do we manage Stevens-Johnson syndrome? We want to remove the offending agent. If it's a medication, we're going to stop it. If it's mycoplasma, we might treat it. We want to provide supportive care such as wound management. These patients do better often in a place that has experience with burns. We need to provide adequate fluid and sometimes fluid hydration is very important in these patients because the skin is denuded and they have a lot of insensible losses and since this condition can take a long time to get better, we need to provide nutrition as well. We need to provide adequate pain management because these patients are in a lot of pain and in particular we want to get the ophthalmologist involved because eye care is critical to prevent any future vision deficit. Lastly, we may try potential adjunctive therapies. Steroids typically do not work. 05:30 People sometimes will try IVIG to try and mitigate somewhat the autoimmune nature of this disease. So that's a quick summary of E. Multiforme and Stevens-Johnson Syndrome. Thanks for your attention.
About the Lecture
The lecture Erythema Multiforme and Stevens-Johnson Syndrome (SJS) in Children by Brian Alverson, MD is from the course Pediatric Dermatology. It contains the following chapters:
- Erythema Multiforme
- Stevens-Johnson Syndrome
Included Quiz Questions
Erythema multiforme is a less common association of which of the following?
- Lymphoma
- Mycoplasma pneumoniae
- Herpes simplex virus
- NSAIDS
- Sulfanamides
Which of the following statements regarding the clinical manifestations of erythema multiforme is TRUE?
- Lesions generally begin as erythematous papules.
- Lesions generally involve flexural areas of the skin.
- Target lesions are rare findings.
- Mucosal membranes are not involved.
- Lesions are asymmetric.
Which of the following groups of drugs is least likely to cause erythema multiforme?
- Antihistamines
- Antiepileptics
- NSAIDs
- Antibiotics
- Sulfonamides
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I feel more confident to recognise these diseases with the clear explanations provided.