Playlist
Show Playlist
Hide Playlist
Upper GI Bleed with Case
-
Slides Gastroenterology 07 Small Intestine Disorders.pdf
-
Download Lecture Overview
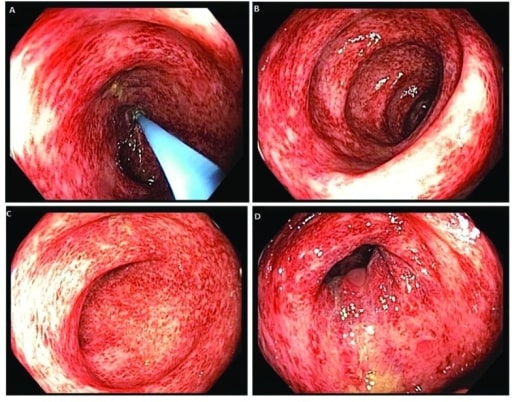
00:01 We'll now start our next case. 00:03 We have a 45-year-old man, seen in the ED for 3 episodes of melena in the last 2 days. 00:10 He has not had any abdominal pain. 00:12 He has no history of bleeding disorders, alcoholism, chronic liver disease or cancer. 00:18 His medical conditions include hypertension and prediabetes. 00:22 This is his first episode of melena. 00:24 He takes high dose aspirin for chronic knee pain. 00:28 His vitals are notable for a heart rate of 110, blood pressure is 125/62 while supine and 99/55 while standing. 00:37 His abdominal exam is unremarkable and rectal exam identifies melena. 00:42 Lab studies show a hemoglobin of 10 but are otherwise normal. 00:47 So what is the best next step in management? Let's go through some key items in this case. 00:53 So he has melena, he has no significant past medical history that would place him at risk for developing melena. 01:01 He does, however, have high dose aspirin use which is a risk factor for GI bleeding. 01:07 And on his exam, this is notable for resting tachycardia, and he has orthostatic hypotension as you note the blood pressure change from supine to standin. 01:17 This indicates that he already has moderate intravascular volume loss. 01:21 So before we answer the question, let's go through a differential for him. 01:27 So as we mentioned in our approach to GI bleeds, there's a very broad differential for upper GI bleeds. 01:34 In this case, if we think through his risk factors, we know that he has a history of chronic NSAID use which puts him at risk for gastric or duodenal ulcers. 01:44 Also, he's at risk for erosive esophagitis, gastritis or duodenitis Although this is rare, he could have an arteriovenous malformation so this should always be on your differential. 01:58 And although he's fairly young, you should always put malignancy on your differential and make sure that you have ruled it out. 02:04 The other causes listed here including esophageal gastric varices or portal hypertensive gastropathy are less likely in him because he does not have a history of cirrhosis. 02:15 In addition, a Mallory-Weiss tear is also pretty unlikely in this case because it does not describe a history of frequent vomiting prior to his bleeding episode. 02:26 So, if we return to our case, we know that he is a 45 year old man,with melena, no particular significant past medical history but he does have high dose NSAID use. 02:37 So the best next step in management includes recognizing that he has moderate hypovolemia so the first step, as always, is to fluid resuscitate and then consult GI for endoscopy. 02:51 Our case now continues. 02:53 The patient is fluid resuscitated, he has no further episodes of melena. 02:58 He undergoes an upper endoscopy which does not visualize a source of bleeding. 03:03 He then undergoes a video capsule endoscopy followed by push enteroscopy as so shown here. 03:10 So first, this is a video capsule endoscopy, so the patient swallow a small capsule that then allows us to visualize the small bowel. 03:20 Here, you see a small amount of bleeding in the jejunum. 03:25 The next step after doing a video capsule is to do push enteroscopy which is a method by which we can then visualize the small bowel which is otherwise very difficult to access. 03:36 So here you see an image from his push enteroscopy that shows a small area of angiodysplasia in the jejunum which probably corresponds to the area that was bleeding on the video capsule. 03:50 And the next step, he then undergoes argon plasma coagulation which is a method of hemostasis to stop the bleeding. 03:58 And after this vessel is coagulated, he then has resolution of his bleeding. 04:04 So let's talk a bit about angiodysplasia or arteriovenous malformations. 04:10 While they are rare, they can cause up to 47% of GI bleeds and they're caused by a vascular abnormality. 04:18 So, as you can see here on the right, normally a capillary bed is made by an arterial and a venule coming together, that's, on top, you can see a normal blood vessel. 04:29 On the bottom on the other hand, these blood vessels may form abnormally and cause an abnormal connection which is an AVM. 04:38 So patients with AVMs may have either overt or occult GI bleeding and usually their bleeding is unmasked by things like aspirin, NSAIDs or anticoagulants. 04:52 The diagnosis as with all GI bleeds is done by endoscopy. 04:58 And with endoscopy, you can also treat. 05:01 So we have various hemostasis interventions to stop the vessel from bleeding including injecting epinephrine, doing coagulation, or placing a clip on the bleeding vessel to stop it from bleeding. 05:17 You might encounter the term "Dieulafoy's lesion". 05:20 A Dieulafoy's lesion is just a particular type of AVM. 05:25 It refers to a dilated abnormal vessel that erodes into the epithelium without causing an ulcer. 05:31 It is usually referred to in the proximal stomach but can really be found anywhere in the GI tract.
About the Lecture
The lecture Upper GI Bleed with Case by Kelley Chuang, MD is from the course Disorders of the Small and Large Intestines.
Included Quiz Questions
Which of the following is the best next step after fluid resuscitation in a patient with melena?
- Endoscopy
- Abdominal X-ray
- Abdominal CT
- Abdominal ultrasonography
- Colonoscopy
Which of the following is the best treatment option for arteriovenous malformations?
- Argon plasma coagulation via endoscopy
- Antibiotics
- Norepinephrine injection
- High-fiber diet
- Anticoagulation
Which of the following terms is used to describe a dilated abnormal vessel that erodes epithelium without causing an ulcer?
- Dieulafoy lesion
- Arteriovenous malformation
- Vascular ectasia
- Hemangioma
- Telangiectasia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |