Playlist
Show Playlist
Hide Playlist
Review of Potassium Metabolism
-
Slides Potassium Disorders Hypo and Hyperkalemia.pdf
-
Download Lecture Overview
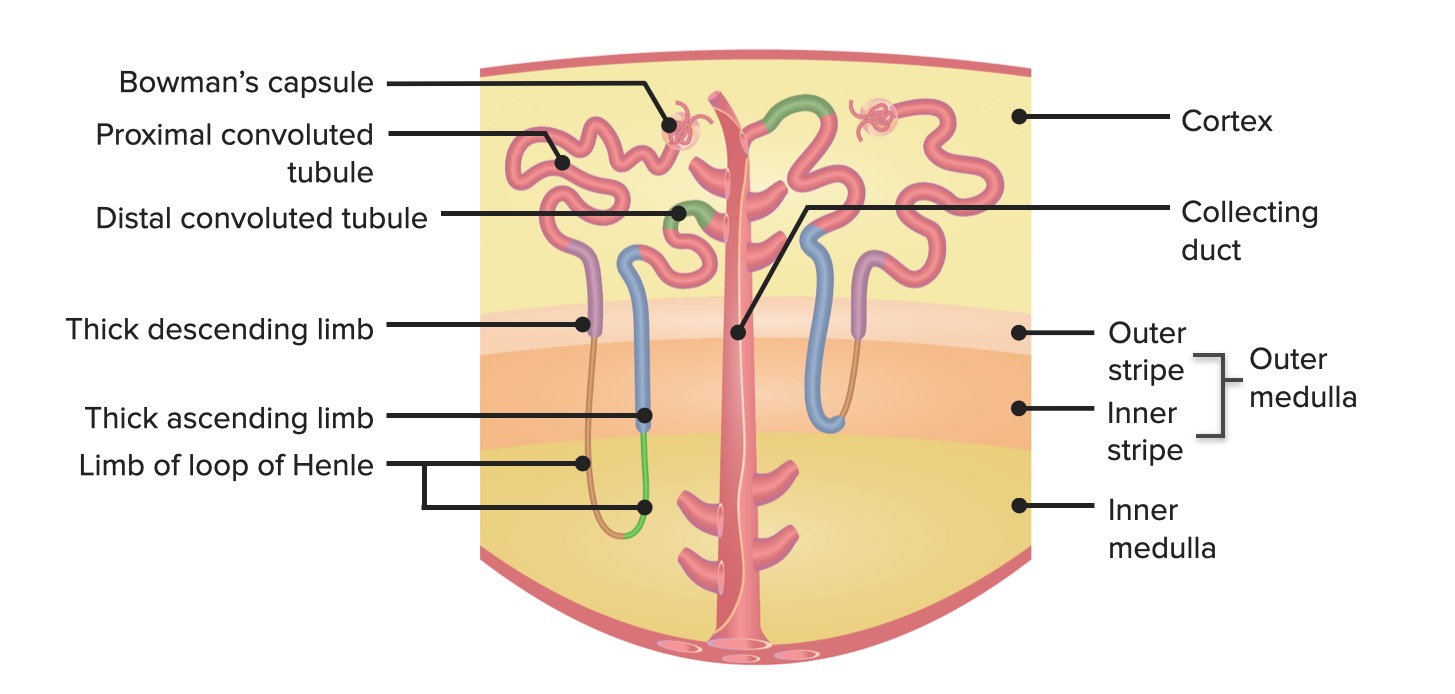
00:01 Hello and welcome back to the nephrology curriculum. 00:04 Today we're going to be talking about potassium disorders and in particular the clinical entities of hypo and hyperkalemia. 00:12 Let's start with the physiology of potassium metabolism. 00:15 So in terms of potassium intake, the average intake in a western diet would be somewhere between 70 and 150 millimoles of potassium per day. 00:24 Now, you might be surprised to see where some of those highest sources of potassium are coming from. 00:28 Look at avocado for instance. 00:30 One medium sized avocado has about 38 millimoles of potassium. 00:34 Tomato paste has a high amount of potassium as well as sirloin steak and some of the meats that we ingest. 00:40 Things like orange juice potatoes and raisins are also very high in potassium and that becomes very important in patients who have to limit their potassium. 00:50 Now once we in take potassium through our diet, it's absorbed efficiently by the GI tract. 00:56 It's then distributed into primarily the intracellular compartment. 01:00 So about 98% of our potassium resides within that intracellular fluid compartment and only 2% is actually distributed to the extracellular fluid compartment. 01:10 The normal plasma potassium, that's what's in that ECF is about 3.5 to 5.2 milliequivalents per liter. 01:18 Now our electrogenical sodium potassium ATPase drives that asymmetrical potassium distribution between that ICF and ECF. 01:27 So remember that sodium potassium pump that's located at those cells. 01:30 It actively transports two potassium ions into the cell in exchange for extrusion of three sodium ions into the extracellular fluid compartment. 01:41 Now that maintenance of that intracellular potassium and that asymmetry between those two compartments is critical for nerve conduction and muscular contraction, so we have to have that. 01:51 When we think about potassium balance, there's four main mechanisms that we really have to remember. 01:57 Number one is the intake that we get through our diet. 01:59 So what are we eating in terms of our potassium. 02:02 Number two is GI losses. 02:04 The GI tract is going to secrete anywhere from 5-10% of our absorbed potassium daily. 02:10 But look at the renal losses 90 to 95% of potassium is really regulated by the kidney. 02:18 And then of course, there's an element of transcellular potassium shift. 02:22 That means that the actual potassium levels are total body potassium is the same but there is a redistribution between the ICF and ECF. 02:31 So we just said that 90 to 95% of potassium is regulated by the kidney. 02:37 Let's take a little tour through our nephron and find out how this occurs. 02:42 So potassium is freely filtered at the glomerulus. 02:46 About 65% to 70% of that filter potassium is going to be reabsorbed in the proximal tubule. 02:53 Now when it's reabsorbed there. 02:54 This is a passive transport process. 02:57 It gets reabsorbed paracellularly, That means between cells by solvent drag and diffusion. 03:03 So this is as opposed or in contrast to active transport, which is what is diagrammed in my top diagram there. 03:11 That's one of my proximal tubular epithelial cells and you can see there's an ion channel and apical transport protein. 03:18 When we have proteins or ions that are actually absorbed through these channels. 03:22 That's an active transport process requiring energy. 03:25 However, the way potassium gets reabsorbed at that proximal tubule is passive, meaning that again, it's moving between the pair cellular pathway between cells and it's going through diffusion and solvent drag. 03:37 An easy way to remember that is P passive transport proximal tubular paracellular. 03:45 Now the next stop in our nephron that's important when it comes to potassium is the thick ascending limb of the loop of henle. 03:52 This area is responsible for reabsorbing about 10 to 25% of potassium. 03:58 And it's driven by our luminol sodium potassium two chloride or NKCC2 Multi Porter. 04:05 Now, this is also the site of loop diuretics. 04:08 It's an active transport process Meaning that this is actually driven by that basolateral sodium-potassium ATPase located on the right. 04:18 Our transporter affinity is going to be very very high for both sodium and potassium and have max activity when the tubular fluid concentration for sodium and potassium or below 5 to 10 Milli equivalents. 04:32 Now, one of the elegant things about this cell is the whole idea of potassium recycling. 04:36 Potassium can actually recycle across that luminol membrane allowing for continued activation of the NKCC2 and that makes sense to us because sodium is in much higher concentration compared to potassium. 04:48 So in order for us to be able to absorb all of the sodium, we would have to recycle that potassium in order to make that transporter work and that's exactly what happens. 04:58 The activity of that potassium channel is actually inhibited by ATP and it allows us to link to the level of sodium reabsorption. 05:06 So as more sodium enters the cell sodium gets transported out of the cell into that peritubular capillary by that sodium potassium ATPase that lowers the cellular ATP level and it stimulates the activity of that luminol potassium channel also called the renal outer medullary potassium channel. 05:26 That will then allow permit the return of reabsorbed potassium into the lumen and then further linked to sodium reabsorption. 05:34 So moving on from the thick ascending limb of the loop of henle. 05:37 The next important stop is in the principal cell. 05:41 Our principal cells are located in that cortical collecting duct, and they have a very important job when it comes to potassium handling. 05:48 So initially potassium is actively transported into that cell by our sodium potassium ATPase at the basolateral membrane. 05:56 It's then secreted into the tubular fluid down of favorable electrochemical gradient by luminal potassium channels and that apical membrane. 06:03 These are governed by factors that affect passive transport. 06:07 So things like a concentration gradient across the luminal membrane think about where potassium is distributed. 06:12 We just said that it's primarily in the intracellular compartment. 06:16 So we have a very high amount of potassium intracellularly a very low amount of potassium in the tubular fluid. 06:21 So it will favor to move or E-flux into that tubular fluid down its concentration gradient. 06:28 We also have an electrical gradient here. 06:30 So that is generated by reabsorption of sodium sodium is going to go to that epithelial sodium channel be reabsorbed into that principle cell when it does so, it leaves a negative charge behind because even though it's paired with sodium chloride chloride gets reabsorbed at a later time. 06:45 So that negative charge then is going to favor potassium reflux in e-flux into that tubular fluid. 06:52 And finally, we have potassium permeability of those luminal membranes. 06:56 So not only are those luminal membranes present. 06:59 They have to be open. 07:01 So with all of these together, these are some of the regulators of potassium excretion in our principal cell. 07:07 Now there's four main factors that you really have to think about when it comes to potassium secretion at that principle cell and I promise you if you remember these four things you will be able to solve any potassium problem that you are ever confronted with. 07:20 The first factor that I want you to think about is aldosterone. 07:24 Aldosterone remember is created by the Zona glomerulosa in the adrenal gland and it's job with regards to potassium is going to be to augment potassium secretion from that principle cell in e-flux that into the tubular fluid. 07:37 It does so by a number of ways. 07:39 1. It increases the number of open sodium channels and potassium channels in that luminal membrane. 07:44 So not only are they there they have to be open. 07:47 It also enhances the activity of the sodium ATPase that basolateral membrane. 07:53 Second factor to think about in terms of what regulates potassium e-fux at the principal cell is plasma potassium. 07:59 If I have a very high plasma potassium, I'm going to need to actually get rid of extra potassium the same mechanism that applies with aldosterone is going to happen here. 08:09 So high potassium levels cause patients to increase the number of open sodium and potassium channels in that luminol membrane and also will enhance the activity of the sodium-potassium ATPase at that basolateral membrane. 08:20 Now, the third factor to think about is the distal flow rate. 08:24 And what that means is the flow of the tubular fluid and how fast it's moving. 08:29 When you have an increase in distal flow rate or increase in tubular fluid rate. 08:33 It's going to watch the secreted potassium away and replace it with relatively low potassium fluid that's going to then favor that concentration gradient. 08:43 It's going to favor potassium moving from the intracellular compartment to the tubular fluid. 08:49 It's going to move down its concentration gradient. 08:52 Now when that distal flow rate is reduced, you're going to have a high luminal potassium content because of less washout and low urine flow. 09:00 So less potassium is going to e-flux into that tubular fluid. 09:05 Now you also there are some other mechanisms that are at play here. 09:09 There are something called Maxi-K channels. 09:11 These are voltage-gated channels that sense that tubular flow rate. 09:14 And again, they will help in the response of potassium e-flux into that tubular fluid. 09:19 So take home point when you have a high tubular fluid rate, so that would be a patient who might be polyurethane meaning that they make greater than 3 liters of fluid that is going to stimulate potassium secretion when you have a low tubular fluid rate meaning somebody who might be oliguric they're going to have less e-flex up potassium into that tubular flow rate and have a higher plasma potassium. 09:42 Now last factor to remember is distal sodium delivery. 09:46 So think about what happens when you have sodium that is presented to that principle cell, you've got entry of sodium by that epithelialsodium channel that makes the lumen electronegative Remember sodium's going to leave behind a negative charge as it gets reabsorbed. 10:01 You then have transport of sodium into the peritubular capillaries by that atpase at the basolateral pump and that's going to pump more potassium into that cell, and then you have more potassium secreted into the electronegative lumen. 10:14 So when we think about distal sodium delivery, that would be the mechanism by which loop diuretics and thiazide diuretics cause hypokalemia. 10:23 They allow for an increase in distal delivery of sodium to this site. 10:29 Our last stop in the nephron, as it pertains to potassium is the alpha intercalated cell at the collecting duct. 10:35 This cell is critical because it reabsorbs potassium and it does it through the apical hydrogen potassium ATPase shown here. 10:42 This is an active transport process meaning that it requires energy. 10:46 So it will actively secrete protons into that tubular lumen or the tubular fluid in exchange for potassium reabsorption. 10:56 The act of reabsorption by that hydrogen ATPase really enables us to be able to reduce our urinary potassium excretion to less than 15 millimoles per day in severe potassium deficiency.
About the Lecture
The lecture Review of Potassium Metabolism by Amy Sussman, MD is from the course Potassium Disorders: Hypo- and Hyperkalemia.
Included Quiz Questions
Which of the following enables the cells in the thick ascending limb to absorb sodium efficiently?
- Potassium recycling
- Increased aquaporin expression
- Inhibition of Na/K ATPase
- Increased epithelial sodium channel (ENaC) sensitivity
Most of the filtered potassium is absorbed in...?
- ...the proximal convoluted tubule.
- ...the thick ascending limb of the loop of Henle.
- ...the principal cells in the collecting duct.
- ...the intercalated cells in the collecting duct.
Which of the following provides the driving force for the active transport of potassium ions?
- Sodium-potassium ATPase
- Na-K-Cl cotransporter (NKCC)
- Renal outer medullary potassium channel
- Hydrogen-potassium ATPase
- Epithelial sodium channel (ENaC)
Which of the following decreases potassium excretion?
- Decreased urine flow rate
- Increased aldosterone release
- Decreased sodium plasma concentration
- Increased distal sodium delivery
- Increased Na/K ATPase activity
What is the mechanism of thiazide-induced hypokalemia?
- Increased distal sodium delivery
- Decreased activity of Na-K-2Cl channels
- Increased activity of Na-Cl cotransporter in the distal tubule
- Decreased urine flow rate
Which of the following is true?
- Severe hypokalemia increases the activity of hydrogen-potassium ATPase.
- Paracellular potassium reabsorption at the proximal tubule is against the electrochemical gradient.
- Aldosterone decreases the activity of luminal potassium channels.
- Of total body potassium, 98% is in the ECF.
- Loop diuretics cause hyperkalemia by increasing the urine flow rate.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |