Playlist
Show Playlist
Hide Playlist
Duodenal Ulcer with Case
-
Slides Gastroenterology 07 Small Intestine Disorders.pdf
-
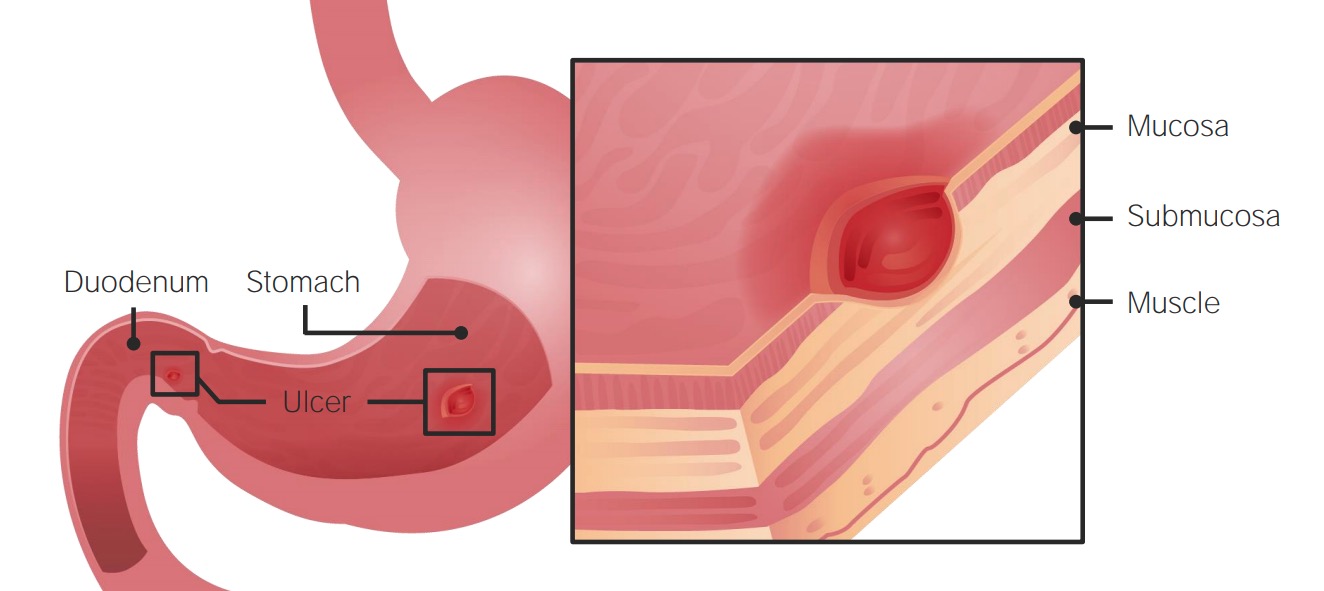
Download Lecture Overview
00:00 Welcome, today we'll be discussing disorders of the small bowel. 00:05 So we'll begin with a case. 00:07 We have a 34-year-old man who presents at the ED complaining of dark stools for the last 2 days. 00:13 He has had epigastric pain for the 2 weeks that improves after eating and is worse at night. 00:19 He has had nausea and a feeling of fullness after eating small amounts. 00:23 He's not had any difficulty swallowing or unintentional weight loss. 00:28 He is a construction worker and takes naproxen several times a day for back pain. 00:33 His vitals are notable for a heart rate of 100. 00:36 On exam, he has mild tenderness to palpation in the epigastrium, without rebound or guarding. 00:43 Rectal exam shows a small amount of black stool in the rectal vault. 00:48 Hemoglobin is 9 from a baseline of 11 several months ago. 00:53 What is the best next step in management? So before we answer that, let's go through some key features here. 00:59 He has dark stools which should prompt you to consider a GI bleed. 01:05 He does have symptoms that are concerning for either peptic or duodenal ulcer disease since he has pain that improves after eating, nausea and early satiety. 01:15 He does have chronic NSAID use. 01:19 And on his exam, he has mild tachycardia. 01:22 When I see a patient who comes in complaining of dark stools, this is often a very vague complaint. 01:28 You always want to do a rectal exam to confirm that it is actually black stool which is positive for melena. 01:35 So in this case, his rectal exam was positive. 01:39 He also has what we consider a subacute hemoglobin drop. 01:43 Meaning, over several months he then had his hemoglobin drop from 11 down to 9. 01:49 So, before we answer this question, let's take a quick step to review some steps in GI bleed management. 01:56 I'll refer you back to the lecture on the approach to the patient with a gastrointestinal bleed for a more in-depth review. 02:03 But we'll go through a quick overview as well. 02:07 So, recall that when managing a GI bleed, the most important steps include establishing adequate IV access with large bore IVs or a centrally placed large bore catheter. 02:20 You then fluid resuscitate the patient and offer blood products. 02:26 So packed red blood cell transfusion if a hemoglobin is less than 7 or you would consider a higher threshold if they are actively bleeding or have cardiovascular disease. 02:36 You may consider giving platelets if their platelets are less than 50,000 and you give medications including a proton pump inhibitor, you might consider vasoactive medications if you're concerned for a variceal bleed, and consider any reversal agents for anticoagulants that your patient is taking. 02:55 The last step is to always consult GI so that they can then do the diagnostic and therapeutic next steps. 03:03 So, let's review duodenal ulcers now. 03:05 Duodenal ulcers are very similar to peptic ulcers. 03:09 They are caused by the same risk factors. 03:11 So those things include H. pylori infection, chronic NSAID use, regular acid hypersecretory states like Zollinger-Ellison syndrome and smoking. 03:23 Patients will come in with the same clinical features as they do with peptic ulcer disease. 03:27 They may have epigastric pain, nausea/vomiting, a feeling of early satiety and unintentional weight loss. 03:34 Here on the right you can see an example of a duodenal ulcer at the bottom of the image. 03:41 The diagnosis must be done with upper endoscopy or esophagogastroduodenoscopy - what we refer to as an EGD. 03:50 You should always make sure to also check for an H. pylori infection since this is easily treated. 03:57 Treatment consist of doing endoscopy and intervening at that point if it's a bleeding ulcer. 04:03 You also need to identify any underlying risk factors and treat those. 04:08 And you may also do a PPI (Proton Pump Inhibitor) or H2 blockers. 04:14 So, you might be wondering at this point, gastric and duodenal ulcers are very similar. 04:20 Some features you can use to distinguish between the two are listed here. 04:25 So first, patients who have gastric ulcers tend to be older or age greater than 40. 04:32 Patients who present with duodenal ulcers on the other hand tend to be a bit younger. 04:38 In addition to risk factors, also differ a bit between the two. 04:41 So for gastric ulcers, the most common cause in developed countries is NSAID use and with duodenal ulcers, H.pylori infection tends to be more common. 04:52 The location obviously differs. 04:54 With gastric ulcers, they tend to occur on the lesser curvature of the stomach whereas duodenal ulcers tend to occur a few centimeters distal to the pylorus. 05:04 Their clinical features may be similar but in general, gastric ulcers, people with gastric ulcers tend to have eating that worsens with pain. 05:14 and those with duodenal ulcers tends to have their pain get relieved by eating. 05:20 They may also more commonly present with nocturnal pain. 05:24 The follow up that is required also differs between the two. 05:28 Because gastric ulcers may have a risk of progressing to cancer, they may require a follow-up endoscopy. 05:35 For duodenal ulcers on the other hand, we often do not need to repeat endoscopy since they have a low risk of progressing to cancer. 05:43 So now let's return to our case. 05:45 We have a 34-year-old man presenting with melena for the last 2 days, concerning for a GI bleed. 05:51 He has chronic NSAID use which is a risk factor for both peptic and duodenal ulcers, although more commonly, peptic ulcers. 05:59 He also has signs of mild hypovolemia based on his rapid heart rate. 06:03 So in a real life situation, if you saw this patient, you would think of both gastric or duodenal ulcers on your differential. 06:11 And the only way to differentiate between the two would be to then perform upper endoscopy to look for the location of the ulcer. 06:19 For test taking purposes on the other hand, if you were faced with a scenario, you should look at the clue that he has pain that improves after eating which is more specific to a duodenal ulcer. 06:30 So because of that, you should recognize that he has duodenal ulcer leading to a GI bleed and the next steps would be fluid resuscitation and performing an EGD to look for the bleeding ulcer.
About the Lecture
The lecture Duodenal Ulcer with Case by Kelley Chuang, MD is from the course Disorders of the Small and Large Intestines.
Included Quiz Questions
Which of the following is true about a duodenal ulcer?
- Eating relieves the pain.
- Eating worsens the pain.
- Constipation is always present.
- Hematemesis is always present.
- NSAID use is the most common risk factor.
Which of the following is the initial step in the management of GI bleeding?
- IV access and fluid resuscitation
- Proton pump inhibitors
- GI consult
- Octreotide
- Anticoagulation
Which of the following is the best diagnostic test for a duodenal ulcer?
- Esophagogastroduodenoscopy (EGD)
- Abdominal CT
- Colonoscopy
- Sigmoidoscopy
- Abdominal ultrasonography
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |