Playlist
Show Playlist
Hide Playlist
Diabetic Ketoacidosis: Pathophysiology, Physical Exam & Diagnosis
-
Emergency Medicine Bord Hypo and Hyperglycemia.pdf
-
Download Lecture Overview
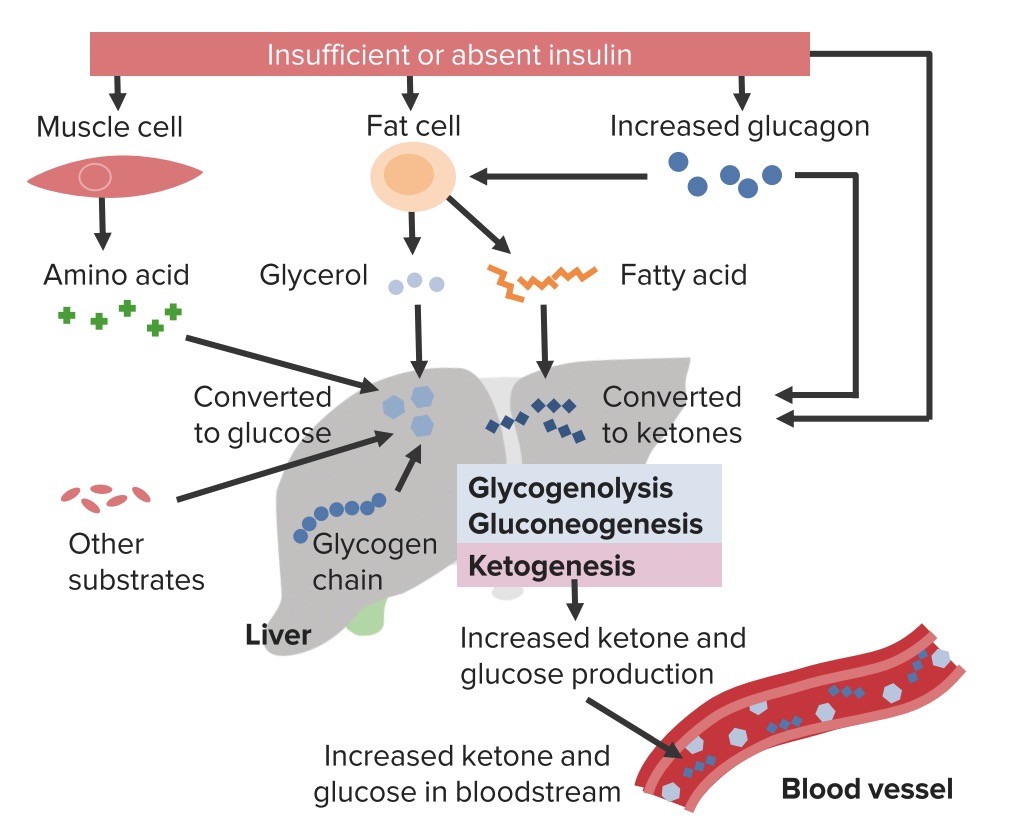
00:01 Next, we’re gonna talk about diabetic ketoacidosis. 00:04 This slide has a lot of information on it and we’re gonna go through it but I want you to focus on what eventually is happening at the bottom of the slide. 00:12 Here’s the pathophysiology of diabetic ketoacidosis. 00:16 So what basically will happen is there’s increased lipolysis and triglyceride breakdown. 00:21 What that means basically is your body is digesting its fats. 00:25 There’s also decreased glucose uptake. 00:29 So the body is gonna be taking up less glucose and there’s increasing breaking down of proteins. 00:34 So over here on this right side, the patient’s gonna have increased free fatty acids which in turn is gonna lead to increased ketogenesis. 00:43 So increased formation of ketones which will in turn lead to acidosis. 00:49 Here in the center here, we see that increased free fatty acids is also gonna lead to hyperglycemia, as will decreased glucose uptake. 00:58 Hyperglycemia is gonna lead to increased glucose in the urine which will in turn lead to more urine production. 01:05 So that’s something that happens in the patients who present even with uncomplicated hyperglycemia. 01:11 This is why patients have polyuria, increased urination when they’re presenting with hyperglycemia. 01:16 And this osmotic diuresis, this increasing loss of urine is gonna lead to volume depletion and electrolyte loss as well. 01:25 In turn, it may lead to impaired renal function which can worsen acidosis. 01:30 You’re also gonna have increasing proteolysis and that’s gonna be increasing amounts of breaking down of the proteins which is gonna lead to increased amino acids, and then increased gluconeogenesis. 01:44 So basically, then the body is gonna be making more glucose, new glucose, which will in turn lead to worsening hyperglycemia and increasing osmotic diuresis. 01:56 So you could see that all of these things play off on each other. 02:00 They all lead to hyperglycemia, they lead to volume loss, and acidosis. 02:05 In addition to patients having polyuria, and polydipsia and polyphagia, patients with DKA will also potentially have weakness. 02:14 They may have blurry vision, nausea and vomiting, and abdominal pain. 02:20 Abdominal pain is a very common presenting symptom in the pediatric patient. 02:25 It’s also important to remember that hyperglycemia can lead to recurrent infections so thrush and candida, as well as Balanitis which is a penile infection. 02:37 So keeping that in mind when you’re evaluating patients with hyperglycemia, it can be helpful to ask if patients have had any kind of fungal infections. 02:47 On the physical exam, you’re looking potentially, your patient may have altered mental status. 02:53 They may be confused and that’s due to the volume depletion, the acidosis, the renal failure. 02:58 A classic thing is Kussmaul respirations. 03:02 What this is, is it’s a rapid breathing, almost like a dog panting after they’ve run a long distance is how I think about this. 03:09 The reason that patients have Kussmaul respirations is because they’re trying to breathe off some of the carbon dioxide, they’re trying to breathe off the acidosis component. 03:18 So they have this rapid breathing. 03:22 You also might note an odor of acetone. 03:25 Now, not everyone can smell this and we’ll get more to that in a moment but there are some physicians who can walk past a room of a patient who’s there with hyperglycemia and say, it smells like ketones. 03:36 I’m not one of them but there are a handful of people who can. 03:40 And then, hypotension and tachycardia. 03:43 The patients may be low blood pressure, they may have elevated heart rate, and that’s due to the diuresis and the volume depletion. 03:52 About 30% of the population can smell acetone on someone’s breath. 03:56 Again, like I said, I’m not one of them, but if you are, consider yourself lucky. 04:00 You’ll have a great benefit when diagnosing patients with diabetic ketoacidosis. 04:05 Now, why do people get this? So new onset diabetes is the cause about one quarter of the time. 04:12 So, these are patients who have not yet been diagnosed with diabetes. 04:16 Oftentimes, this is in a pediatric patient or a younger patient who’s presenting. 04:20 You always wanna be thinking about other underlying causes or reasons because DKA is commonly caused by something else. 04:29 Infection or sepsis is a common one. 04:32 So when you have patients coming in with DKA, you can’t just stop there and say, “Oh, it’s DKA, we’re done.” You have to be thinking about what could potentially be causing it. 04:41 Cardiac causes are another. 04:43 Myocardial ischemia can definitely lead to DKA. 04:47 There are also emotional stressors. 04:49 So patients who are under a lot of financial, legal, family stress can lead to this. 04:56 And then, medication non-compliance. 04:59 Patients all the time decide not to take their medication for various reasons. 05:04 They can’t afford their medicine. 05:05 This is common in like a female teenage patient who recognizes that if she doesn’t take her medication, she can actually lose weight. 05:13 So this is not uncommon for that specific patient population that they don’t take their medication. 05:19 So medication non-compliance is a big one. 05:21 I’ve taken care of patients multiple times who present with the exact same complaint with DKA or the exact same diagnosis mainly because they just didn’t take their medicine. 05:32 So thinking about the diagnosis. 05:36 D stands for diabetes. 05:38 So what this means is that you’re going to have an elevated blood sugar. 05:41 Generally, it’s greater than 350 mg per deciliter but you can also have this concept of euglycemic DKA which is when you have DKA where the blood sugar is less than 300. 05:53 K stands for ketosis. 05:56 So the body is forming ketones. 05:59 And A stands for acidosis. 06:02 Now, this is an anion gap metabolic acidosis. 06:05 So this falls into the differential for anion gap metabolic acidosis. 06:09 You probably remember the mnemonic MUDPILES. 06:12 So M stands for Methanol, U, Uremia, D for DKA, and we can go through the rest of the mnemonic at another time. 06:20 So D is our DKA component here. 06:22 For these patients, a chemistry and a venous blood gas will help diagnosis that acidosis component. 06:29 So you’re looking for a low pH on your venous blood gas and on your chemistry, you’re looking for a low bicarbonate level. 06:36 These patients are acidotic. 06:38 For DKA, arterial and venous blood gas pH measurements correlate very, very closely. 06:46 So the only reason that you would need to get an arterial blood gas would be if you were concerned about oxygenation or some kind of respiratory issue but for the most part, a venous blood gas will be an appropriate and adequate test when you’re worried about the acidosis. 07:01 It’s important that we take a moment to think about some electrolyte issues that we’re gonna see in DKA. 07:08 So the first is sodium. 07:10 Patients with DKA and with hyperglycemia in general can get something called pseudohyponatremia. 07:16 What this basically means is that the sodium level actually is okay in the blood but what’s being reflected in the labs is inaccurate. 07:25 So we can do a calculation to correct for this phenomenon and the calculation is that you add 1.6 milliequivalents per liter to the sodium value on the lab report for every 100 mg per deciliter of glucose that are above the norm. 07:41 So what you’re doing is you’re correcting your sodium level. 07:44 Next, potassium, magnesium, and phosphorus. 07:48 Now, it’s important to remember that overall, you’re gonna have total body depletion of these electrolytes. 07:55 So your body is actually gonna be deplete of them but the level may be normal or elevated. 08:00 One of the big reasons for potassium is that on the cells, there’s a potassium/hydrogen exchange channel. 08:07 And what happens when hydrogen ions are high as in a state of acidosis, the potassium is gonna go into the cell or out of the cell rather, and the hydrogen ion is gonna go into the cell. 08:18 So the potassium is gonna come out, hydrogen ion in. 08:23 So even if your body is low in potassium, it’s gonna be reflected in the extracellular environment that the potassium may be normal or high. 08:32 The other thing you can get to screen for these electrolyte issues is an EKG. 08:38 So if you’re worried about it, an initial test for DKA to help evaluate for electrolytes and electrolyte abnormalities would be an EKG. 08:48 We’ll be talking more about the EKG changes associated with potassium issues in another lecture. 08:55 The potassium level varies in patients with D K A, as the acidosis may cause intracellular shift of the hydrogen ions in replace of extracellular shifting of potassium ions. 09:08 This causes initial hyperkalemia although the total body potassium level is depleted, therefore continuous assessment of the potassium level is important. 09:19 D K A also causes dehydration which may increase the serum osmolarity to greater than 300.
About the Lecture
The lecture Diabetic Ketoacidosis: Pathophysiology, Physical Exam & Diagnosis by Sharon Bord, MD is from the course Endocrine and Electrolyte Emergencies. It contains the following chapters:
- Diabetic Ketoacidosis Pathophysiology
- DKA: Physical Exam and Diagnosis
Included Quiz Questions
Which of the following processes in diabetic ketoacidosis contributes to increased gluconeogenesis?
- Increased proteolysis
- Decreased glucose synthesis
- Decreased lipolysis
- Increased ketogenesis
- Decreased free fatty acid release
What type of breathing pattern is classically seen in patients with diabetic ketoacidosis?
- Kussmaul respiration
- Cheyne-Stokes breathing
- Biot's breathing
- Ataxic breathing
- Bradypnea
What is the most common cause of DKA in the pediatric setting?
- New-onset diabetes
- Infection or sepsis
- Medication non-compliance
- Emotional stressors
- Cardiac causes
What electrolyte may be falsely decreased in patients with hyperglycemia or DKA?
- Sodium
- Potassium
- Calcium
- Magnesium
- Phosphorus
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
clear explanation and very good presentations. I love how she explains the causes and the pathophysiology
The reason I rate this as 5 stars is because it was a simple, concrete, and very useful way to remember the key points on DKA at the emergency department that is often full of patients. I'm writing from Colombia.