Playlist
Show Playlist
Hide Playlist
Hypercalcemia and Review of Calcium Homeostasis
-
Slides Calcium Metabolis.pdf
-
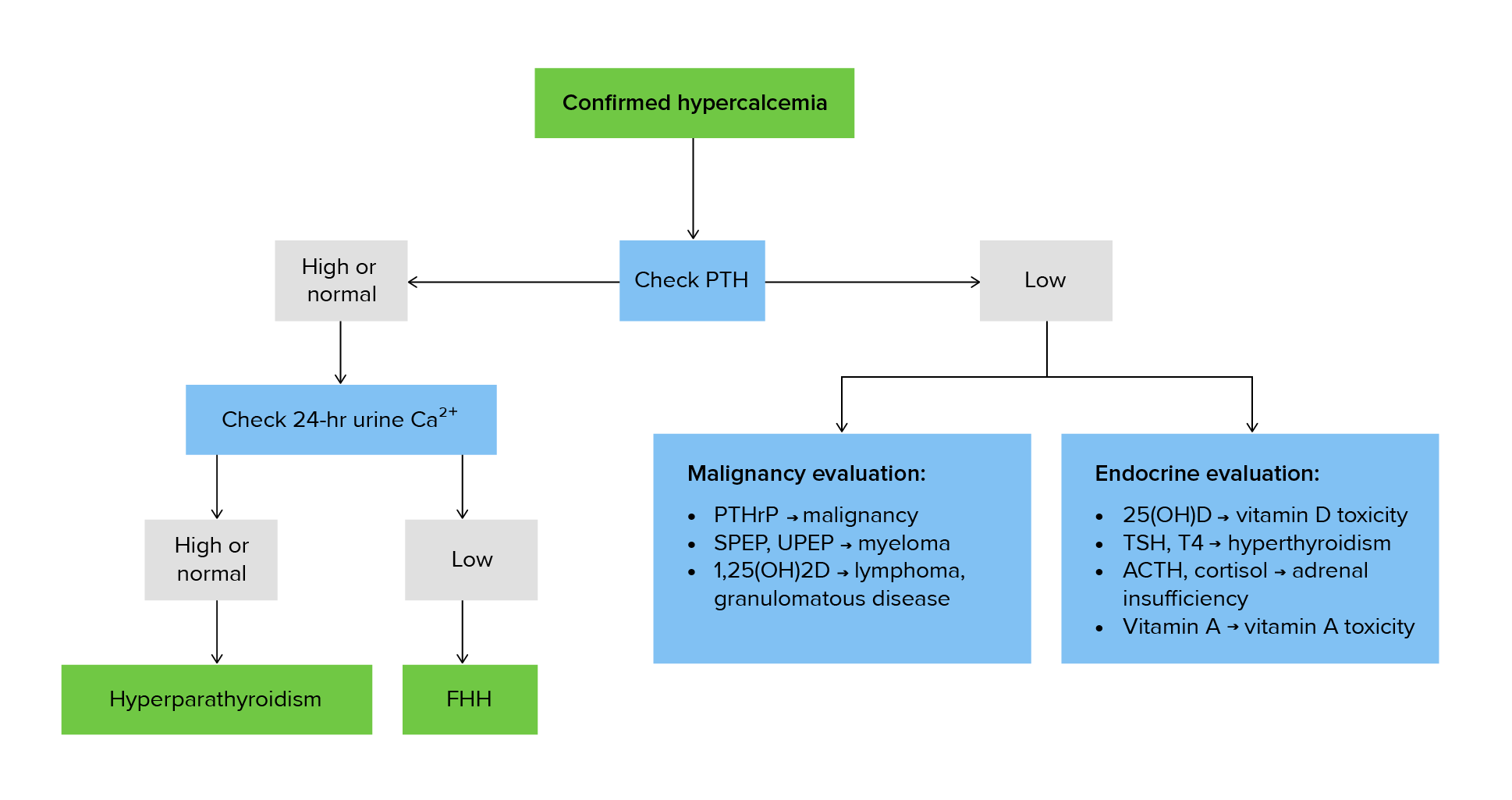
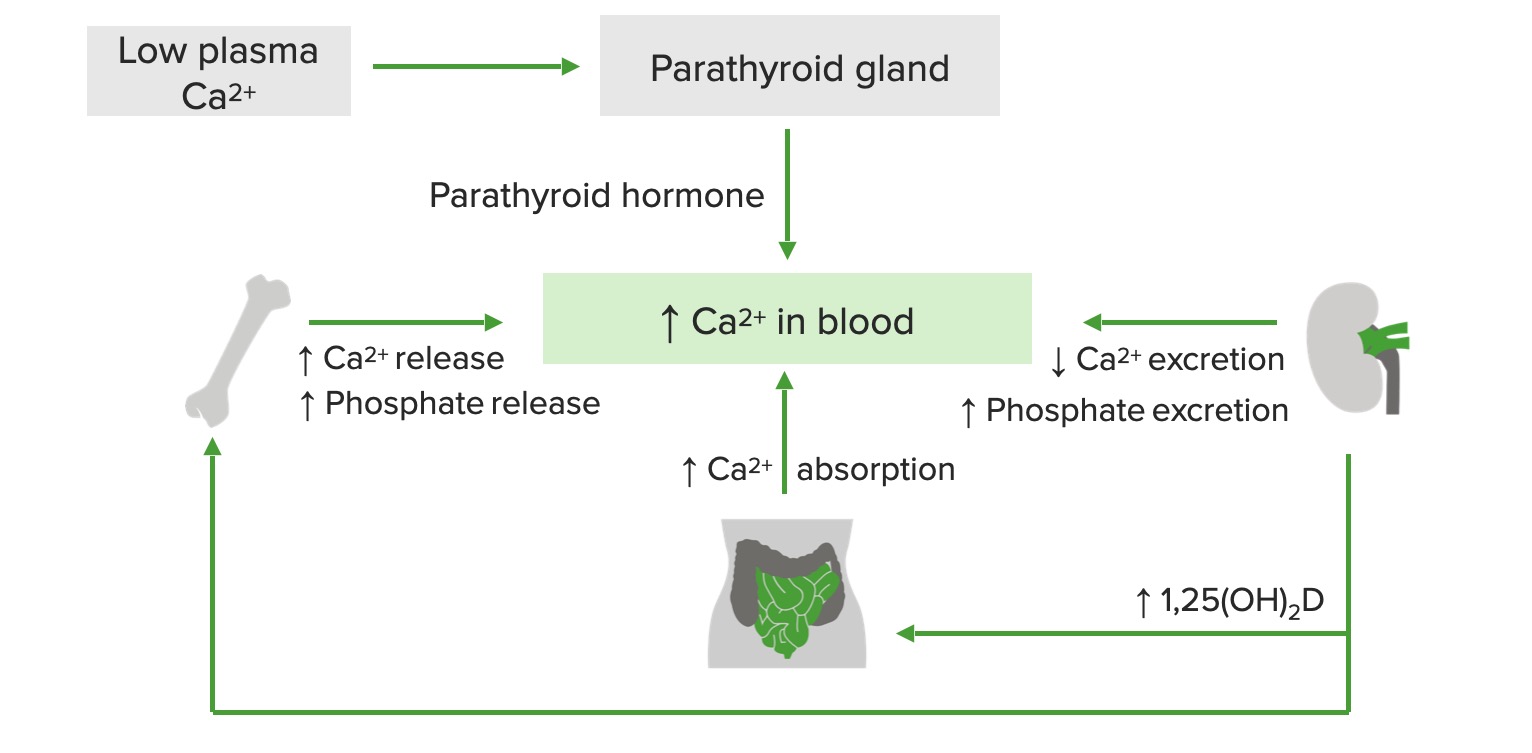
Download Lecture Overview
00:01 Today we're gonna talk about calcium metabolism from an endocrinologist perspective. 00:06 Let's talk with some revision of calcium homeostasis in bone physiology. 00:10 Serum calcium levels are tightly regulated on a moment to moment basis by the actions of vitamin D and parathyroid hormone. 00:20 The amount of calcium that is albumin-bound can be affected by hydration and nutritional status. 00:27 When the albumin levels decrease, the total serum calcium levels may appear low and this is known as pseudohypocalcemia. 00:35 When the albumin levels increase, total serum calcium levels will appear elevated and this is known as pseudohypercalcemia. 00:44 In both cases, by checking an ionized calcium level, you will gain, you will see a normal level indicating that there are normal circulating free levels of calcium. 00:55 The causes of pseudohypercalcemia include conditions that increase protein states within the body, multiple myeloma where there is an elevation of monoclonal immunoglobulins, hyperalbuminemia from numerous causes, Waldenstrom macroglobulinemia which is a hematologic disorder, and thrombocytosis where there is an elevation of platelets. 01:19 The sources of vitamin D which is a fat soluble vitamin, include de novo production in the skin from sunlight, in the food that we eat and also from taking vitamin supplements. 01:32 There are 2 forms of vitamin D supplementation. 01:35 Vitamin D2, also know as ergocalciferol, which has a longer half-life and vitamin D3 or cholecalciferol, which has tighter bonding to vitamin D receptors. 01:46 It also has a greater potency than vitamin D2. 01:50 It's also identical to the vitamin D that naturally occurs in humans after ultraviolet light exposure. 01:57 Vitamin D3 and D2 must be hydroxylated twice before becoming active. 02:02 The first occurs in the liver and converts vitamin D to 25-hydroxy vitamin D, otherwise known as calcidiol. 02:09 The second occurs primarily in the kidney and forms the physiologically active 1,25 dihydroxyvitamin D, otherwise known as calcitriol. 02:20 Because 25-hydroxyvitamin D has a relatively long half-life of several weeks, it is the best indicator of the whole body stores of vitamin D. 02:31 Active vitamin D acts on three organ systems to achieve and maintain normal serum calcium: bone, intestine and kidney. 02:41 PTH is secreted to increase the calcium in the blood in response to even the slightest degree of hypocalcemia. 02:49 PTH acts on the kidney to increase production of active vitamin D to promote calcium resorption in the distal convuluted tubule and the loop of Henle. 02:59 PTH acts on bone to activate calcium and release it into the blood stream. 03:05 The clinical features of hypercalcemia occur when serum calcium levels are above the normal range usually greater than 10.5 mg/dL. 03:15 Most patients are asymptomatic and hypercalcemia may be noted incidentally on lab tests obtained for other reasons. 03:25 Symptoms may occur with any degree of hypercalcemia but they are much more common when calcium levels exceed 12 mg/dL. 03:34 There's a really good way to remember the clinical findings in symptoms that occur in hypercalcemia. 03:41 Stones refers to calcium levels being elevated causing kidney stones. 03:48 Abdominal groans are feature of hypercalcemia and that patients tend to present with nonspecific abdominal pain. 03:56 Bones are reminded that because of elevated levels of PTH, the bones are the primary source of calcium breakdown that enters into the blood stream to cause hypercalcemia. 04:07 And finally, the presence of elevated calcium as it increases causes mood disturbances and ultimately other central nervous system effects. 04:19 The classic symptoms are usually based on the severity of calcium rise. 04:24 So starting at the calcium level of around 11 mg/dL, one notices the classical features of polyuria, polydipsia, nocturia which is increased urination at night and the presence of kidney stones. 04:38 As the calcium levels increase above 11, patients may manifest anorexia, nausea, abdominal pain, constipation. 04:48 There may also be effects on the kidneys. 04:51 The creatinine may rise because elevations of calcium cause what we know as calciuresis or an increased diuresis of water that the body loses causing a prerenal state and hence a rise in creatinine levels. 05:06 This can also be followed with some mild mental status changes. 05:11 And then finally, as the calcium increases above 12, patients present with profound mental status changes. 05:17 They may be obtunded and kidney injury due to profound dehydration may be a manifestation. 05:23 One will also note an increase in creatinine level at this stage. 05:28 The causes of hypercalcemia can be divided into parathyroid mediated and non parathyroid mediated. 05:35 Parathyroid mediated causes are typically those caused by elevations in parathyroid hormone. 05:41 Primary hyperparthyroidism usually caused by an adenoma or increased hyperplasia of the parathyroid gland is the most common cause. 05:50 Parathyroid cancers although very, very rare may cause it and tertiary hyperparathyroidism which is a rare condition that occurs in patients with chronic kidney failure. 06:01 And then finally, the even rarer familial hypocalciuric hypercalcemia which we will discuss later. 06:09 Moving on to non-parathyroid mediated causes of hypercalcemia, Hypocalcemia of malignancy, otherwise known as humoral hypercalcemia is a condition where an abnormal parathyroid hormone is secreted, causing elevations of calcium and usually from bone sources that are related to tumors. 06:29 This is usually a paraneoplastic manifestation. 06:32 Another malignant manifestation of hypercalcemia are those tumors that metastasize to bone and cause bone destruction. 06:40 These can cause calcium release into the bloodstream and mainly because of osteolysis of bone. 06:47 Another common cause of non-parathyroid mediated hypercalcemia is vitamin D toxicity. 06:54 These are individuals who take excessive levels of vitamin D, causing increased calcium absorption and hypercalcemia. 07:01 It is also seen but to a rarer degree with high levels of vitamin A. 07:08 Granulomatous diseases like sarcoidosis and TB also cause hypercalcemia but these are usually mediated through vitamin D mechanisms that we'll talk about later. 07:20 Rarer conditions like milk alkali syndrome, thyrotoxicosis and prolonged immobilization can also cause elevations of serum calcium.
About the Lecture
The lecture Hypercalcemia and Review of Calcium Homeostasis by Michael Lazarus, MD is from the course Metabolic Bone Disorders.
Included Quiz Questions
Serum calcium levels in the body are mainly regulated by which of the following?
- Parathyroid hormone, calcitonin, and vitamin D
- Parathyroid hormone and vitamin A
- Sodium levels and vitamin D
- Parathyroid hormone and vitamin E
- Calcitonin and vitamin A
Physiologically active vitamin D is formed in which organ of the body?
- Kidneys
- Lungs
- Liver
- Bones
- Intestines
Which of the following serum calcium levels best indicates hypercalcemia?
- Above 10.5 mg/dL
- Above 6.2 mg/dL
- Above 3.5 mg/dL
- Above 5 mg/dL
- Above 8.5 mg/dL
Which of the following is NOT a manifestation of hypercalcemia?
- Carpopedal spasms
- Constipation
- Confusion
- Abdominal pain
- Acute kidney injury
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
All the important stuff covered without going too in-depth and overcomplicating it.