Playlist
Show Playlist
Hide Playlist
Extracellular Fluid (ECF) and Intracellular Fluid (ICF): Clinical Volume Dynamics
-
Slides WaterandSodiumPathophysiology RenalPathology.pdf
-
Download Lecture Overview
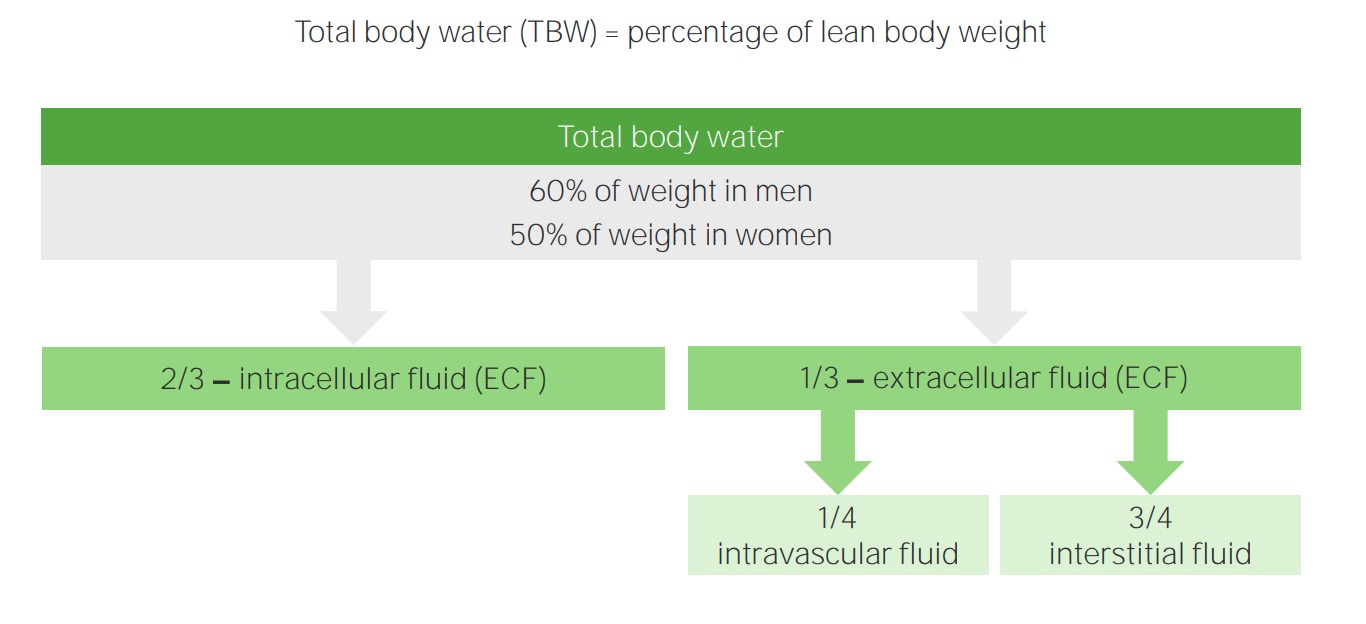
00:00 This is an important table and before begin, though, let me set up the topic. First and foremost, understand what is this saying. Do not breeze past the topic. The effective circulating volume, stop there. You see that. Effective circulating volume, what does that mean to you? Is that the ICF? No. Is that part of the ECF? Yes. It is part of the ECF. So what part is this? What is the effective circulating component of your ECF? Plasma, good. So here all we are dealing with is the plasma compartment when we say effective circulating volume. 00:42 Is that a typo? This does not equal an excess fluid volume? No, it's not, not a typo. It is absolutely accurate. You can have a decrease in effective circulating volume and not at all be equal to the decrease in extracellular fluid ECF and we'll go through examples where that becomes very true. So what does ECF mean to you? ECF is a combination of plasma and interstitium. 01:13 For example, is it possible that you might have an increase in ECF and a decrease in effective circulating volume? That were a rhetorical question. Of course. Example, oncotic pressure is decreased secondary to cirrhosis, congestive heart failure resulting in increased hydrostatic pressure. What did I just say? Liver has been damaged, you don't have enough protein, decrease oncotic pressure. Example number 1, clinically. Example number 2, congestive heart failure, hydrostatic pressure and so therefore where is that fluid moving? From the effective circulating volume, which is not decreased, into the interstitium. So what happen to ECF? It has increased, now you see it clinically. Because if we just rush pass through this, all you done is either not paid attention or you just memorized it and it does not stick. Now on this table, we will go through each one of these examples so that you can clearly see this. The overall theme for this table as you see is decreased effective circulating volume. Let us take a look at the first column here, decreased extracellular fluid volume. Take a look at the concept for the slide, which is the difference between what we call ECV, effective circulating volume, and ECF, extracellular fluid volume, okay. I am going to keep repeating this so you are not confused. The entire theme for this table is decreased effective circulating volume. What is this? The plasma only. So here let us say that you do have volume depletion due to hemorrhage. Got into an accident and there has been a laceration in which there is massive loss of blood. What happens to extracellular fluid? Decreased. See the first column. That is ECF, but what about ECV? Obviously decreased as well because you have lost all blood hemorrhagically externally. There it is on the floor. You see a lot of blood. Oh! My goodness, I miss you so much. So now that is hemorrhage that dramatic enough for you. 03:26 So you have a decrease in ECF and you have a decrease in ECV. 03:30 Next point, a normal ECF and decreased ECV, what is going on here? It is a sepsis. 03:40 In sepsis, what are you thinking? Organism from microbiology? Good. A gram negative organism. 03:43 For example, if a female was pregnant and her urethra is rather small, she is now exposed and she is vulnerable to infection such as E. coli. Here comes the E. coli and it starts to mountain climbing up the female's urethra. Pleasant topic. And eventually, at some point maybe there is pyelonephritis, oh! my goodness, this E. coli and the urinary tract infection and pyelonephritis wasn't properly discovered, ends up resulting with septicemia, eventually result in sepsis. This gram-negative organism with lipopolysaccride, I am going through this quickly because this is micro. The lipopolysacchride and such then brings about all the cytokine changes in which what then happens to our blood vessel? Vasodilation and so now you will have normal extracellular fluid volume, but then you have a decreased ECV because things are moving through this so quickly and there is every possibility that some of this fluid might just be able to move through, increased permeable capillaries. But overall though, with normal ECF clinically with a decrease in effective circulating volume. 04:55 Let us go to the third column. Here this is the one that I mentioned to you earlier with CHF, cirrhosis and nephrotic, put all three together. Congestive heart failure, what is my problem? I want you to focus about right-sided heart failure to make it easier for us and I am going to be more specific here because you must understand the only time that you would find peripheral edema and positive JVD is what kind of heart failure? Right-sided heart failure. Are we clear? Don't ever miss that question. So right-sided heart failure, what are you going to do? Increase hydrostatic pressure, where is this fluid moving from? From the plasma, which we call what? Effective circulating volume into the interstitium, which is part of your ECF. So, therefore, can we clearly see as to how you are going to rapidly, I mean literally you can see the patient with pitting edema. You can clearly see as to how fluid is accumulating in the interstitium in excess. ECF is increasing and how can you confirm that the effective circulating volume is decreased because who is being released from the juxtaglomerular apparatus of the kidney? Renin. How is that possible? Effective circulating volume is decreased. Talked about CHF. What about cirrhosis? We have done this a few times. 06:15 If the liver has been knocked out, then what happens to protein content? You never produce the albumin. What happens to oncotic pressure? It is decreased. Where is my fluid? Good. 06:26 Into the interstitium. How can you confirm that? Look at the patient with cirrhosis. 06:30 Drink too much alcohol for years and years and years and what happened? I used to be in shape once upon a time, but now let us say you are a rock star and maybe perhaps I am just being stereotypical here and I went through a period where I was drinking quite a bit, and then all of a sudden now I sing like this. I can't even see my feet anymore because of my ascites, right. Cirrhosis, what does this mean? Increase in extracellular fluid volume. Are we clear? And what about nephrotic? Most common cause of nephrotic in a child, you will tell me minimal change disease. What do you know about that child losing lots of protein? Losing lots of protein. How much, the magic number? Greater than 3.5 grams of protein per day. What happens to your oncotic pressure? It decreases. Where is my fluid? In the interstitium. Could this table be any more clinical than what it is now? You see the clear difference between effective circulating volume and ECF. If you haven't, you do now. 07:40 Let us move on. 07:44 Quickly go through some important physiologic changes and give it a clinical application with a Darrow Yannet box . First and foremost, this box that we are seeing, I've set it up for you, X-axis. If you haven't done it like this, do it now because your life becomes so much easier. 07:58 The X-axis represents the volume. The Y-axis represents the osmolarity. We have a line in the middle there. That is the barrier and that is separating the ECF and ICF. You tell me what membrane that is. Close your eyes. Be careful. It will come out your mouth. Okay. 08:15 You are thinking one thing, but something else might either come out of your mouth or you might accidentally choose it as being the answer to it. Doesn't it happen all the time? You go back and take a look at a question and you are like why in the world did I choose that answer. So let us avoid all of that. Be deliberate with everything that you do. 08:31 So that barrier and that membrane that you are seeing there ladies and gentleman is which one? Is that the cell membrane or is that the capillary membrane? That is going to be your cell membrane. Good. And tell me about what it's permeant to? Really water, that is about it. Sodium? No, not the cell membrane. Are you kidding me? But Dr. Raj, your sodium channels. 08:52 Would you stop being so hard on me? Yeah, that sodium channel is not open. Understand that. 08:58 If that sodium channel is never opened, you will not permeant to sodium. Clear? It is that clear. It should be. It has to be. Otherwise, your life becomes much more difficult and you don't like that. Next, we are going to go through volume contraction. 09:14 Now the steps that we had initiated a little while ago was the following. So far, the first thing that you want to do always, is always take a look at what kind of change that I have in my plasma compartment, which is part of your ECF. And if that plasma compartment has decreased for whatever reason, just take a look at diarrhea, a wonderful topic. So when there is a loss of fluid, you have ECF volume decreasing. Point number 1. Let me show this to you here. The original black square that you are seeing is being a solid line represents normal, kind of like what we started off originally with the control. The dash line that you are seeing is going to be the change. Here specifically in diarrhea, I do not recommend that you memorize this. 10:10 You use these boxes as a conceptual tool in your head so that when an attending or when you are doing your rounds in the hospital or you are taking a board exam, when people pose questions to you, you have this image in your head so that you can quickly come up with the proper management of your patient. So in diarrhea, you have lost obviously fluid. 10:33 Your ECF volume is going to decrease and what axis here represents the volume? The X-axis. 10:40 Do you see ladies and gentleman that on the X-axis, for the ECF, its volume has decreased? That is your step number 1, always. 10:50 Next, what are you going to do? Well depending as to what kind of loss that you have had. 10:58 You are going to have either an increase, a decrease or no change with ECF. osmolarity. 11:07 Where is my osmolarity on this box, graph? It is on the Y-axis. You'll notice ladies and gentleman with diarrhea that there is basically no change on the Y-axis. So your ECF osmolarity remains normal. I doubt diarrhea is what we're doing here and so, therefore, the type of fluid that you have lost here without any change in ECF osmolarity. What does this have to be? What kind of loss? Good. Isotonic loss, okay. So we will go through the details. All I am doing here is just setting up the picture so that when the time is right and we go through details, we will be able to go through the material efficiently. Let us go to the middle one. 11:49 The middle one, our overall theme for this section is volume contraction and by volume contraction, what do you begin first always? That will be the ECF. Now you will go as far as you need to say get your answer right. So let us go a little bit further here. 12:07 Say it is water deprivation. What does that mean? That means that the individual is deprived of water. 12:13 Why? Well, I'll give you an example. For example, if there's psychogenic polydipsia, your primary polydipsia, what is the one of the first steps that you will do conservatively? You deprived the patient of your water. But what if your patient is crazy? I'm seeing things, I'm hearing things, auditory hallucination. 12:27 That is a psychosis. It is called a psychogenic polydipsia. That patient feels as though he or she needs to be drinking all the time. You restrain that patient okay. 12:35 You have to do water deprivation does. What is my point? What is the water deprivation test? What is the first thing that is going to happen? I am not drinking water anymore. So, therefore, step number 1, ECF volume is going to decrease. You are depriving your patient of water. ECF volume decreases, number 1. So what can you expect your ECF osmolarity to do? As long as everything is normal, your ECF osmolarity should increase now. Take a look at that dash line in the middle picture with water deprivation. Do you see the dash line? And its ECF. Where is my osmolarity? Y-axis. You see it rising. So now you have ECF osmolarity, which is now increased. That is step number 2, always. Now who is going to be influenced and who is going to be affected? The ICF. Tell me about the movement of water across what membrane is this? Cell membrane. The movement of water across the cell membrane. It goes from what kind of movement? Diffusion. It will from a place of low solute to high solute. Correct. 13:37 That is osmosis. Where is your high solute right now? In the ECF compartment. How can you confirm that? The ECF osmolarity. What happen to your patient? Water deprivation. So far so good. You are asking right questions and you're come out with the proper solutions. 13:54 So, therefore, ICF, the water is being pulled out into the ECF. What is step number 3 here? It is the fact that ICF volume is decreased. I can confirm that. Now take a look at ICF. 14:06 Take a look at the X-axis and take a look at the dash line. We will notice that the ICF volume has now diminished. Step number 3, as ICF and its fluid is shifting into the ECF, what is your fourth and final step which we are now covering for the first time? It is a fact that ICF osmolarity has increased. How can you confirm that? Take a look at the dash line and on the Y-axis, you find that to be risen as well. Okay. What are my steps? ECF volume, ECF osmolarity. ICF volume , ICF osmolarity. Prime example while deprivation, we needed all four here. Why didn't we need all this for diarrhea? Because you lost what kind of fluid? Isotonic fluid. Diarrhea out it comes from your butt right and so, therefore, isotonic loss all that you have affected is ECF volume. Stop, that is all you have to do. 14:58 Why create more work for yourself? So be smart about how you approach each patient, each question. Let us move on to adrenal insufficiency. 15:08 Now this one is a little tricker, but I know you can do this, in fact you have no choice. 15:13 So adrenal insufficiency, what then happens here? Good. My question is, who has been knocked out? The adrenal cortex. Primary adrenal insufficiency, give me the proper clinical name. Mr. Addison right, Addison's disease is what this is. Good. In Addison's disease, adrenals are not working properly. If you are dealing with volume, would you tell me what hormone is in play? This has nothing to do with cortisol. Okay. Let that go right now. When the time was right, of course, we will talk further about that. Right now, it is aldosterone that is not present right. The entire adrenal cortex has been destroyed, how? Maybe autoimmune disease. Okay maybe idiopathic, what have you? So now you don't have aldosterone. Work with me. Remember all those discussions of aldosterone that we have had up until now. That's gonna come into play. In adrenal insufficiency we don’t have aldosterone so therefore down the collecting duct, you cannot reabsorb sodium and so therefore it remains within my collecting duct. So therefore what you are losing? Lots of sodium. Lots of sodium is being lost and along with sodium what is it going to do? It is going to pull water out too. Fascinating. So losing all this volume, what's your first step always? ECF volume. Take a look. Where is my volume? X-axis. Good. Take a look at ECF. ECF volume is decreased. Excellent Stop, why? Need you to think okay. Please think. Watch this. You are losing lots of sodium. Where? Into the toilet. There it is. It is my sodium being flushed down the toilet. It is not in my plasma. So tell me about your plasma osmolarity when you are flushing your sodium down your toilet. What's your step number 2? ECF osmolarity. Why is it decreased? Because you are flushing your sodium down the toilet. You see that. Interesting. Compare this to water deprivation. Compare this to diarrhea. We will compare this to a lot. So here you are losing your urine. Fine. You are losing lots of sodium. You find that your ECF osmolarity has decreased. Take a look at the dash line please. Take a look at the Y-axis. You see that to be decreased as well. 17:33 We're at next step number 2. You tell me. What was your third step? ICF volume, good. So now you have a decrease in ECF osmolarity. Which way does your water want to go? Where is your more solute? In the ICF, right. Good. Water is going to shift into ICF. So what happens to ICF volume? Now do you see how things have become easier? ICF volume has increased. How can you confirm that? Take a look at the X-axis and you find the dash line, the ICF volume has increased. 18:00 That is step number 3. And finally as more volume and fluid in my ICF, what would happen to my ICF osmolarity? Good. Y-axis, it is decreased. You see this. You firmly implant these concepts of these boxes with those four steps every single time. There is no way. At least you will be able to get the foundation and then from that you can administer proper management. 18:27 Now the bottom portion here is going to be volume expansion obviously we are not going to spend as much time going through every step. So I'm going to fly thorugh this, but you will be able to stick with me. Ready. The only way you want to do this is you have understood everything up until now. Let's do infusion of strict isotonic saline. Isotonic saline. What is the only thing that is going to happen? Here's your patient, what did he or she suffer from? Hypovolemia and as soon as your patient comes in, what are you going to give? Isotonic saline IV fluid. Step number 1, ECF volume increased. You are done. I don't even care about the other steps right now. Let it go. Let us go to high NaCl intake. 19:11 What is this? Maybe patient taking antibiotics. What is NaCl? No. Listen. High salt only. What is the difference between high salt versus the first one? Take a look at the terminology. Isotonic saline is IV fluids. Strict NaCl is only salt tablets. If all that you are doing is strictly putting salt into the system, what are you going to do immediately? ECF osmolarity increased, thus it is going to pull the water out and as which we are seeing here, you are done. Let us move on to SIADH. 19:52 SIADH could be a little tricky, but you are good. I'm going to give you some examples. Let your patient has had a posterior pituitary issue in which there is producing too much ADH maybe a patient has small cell lung cancer. Small cell lung cancer of what? The lung. And you are releasing too much ADH parineoplastically and you have too much ADH, what then happens? Step number 1, pulling too much water out of your collecting duct, strictly, what kind of water? Is that free or obligated, please? Free. If you are pulling water out, what happens to your ECF volume? Step number 1, increased. Step number 2, ECF osmolarity decreased. Step number 3, what is going into the cell? ICF volume, increased. Step number 4, ICF osmolarity, decreased. You must do that quickly and you will get there if you haven’t already. Fantastic. Let us move on. Now after that, things become more interesting clinically, okay. What I wish for you to focus upon here is the same box the same issues in terms of the X-axis, Y-axis? I am not going to cover that again, but what I wish to cover is D5W. Okay. What does that mean to you and when would you even think about giving this? D5W is strict pure water. Dr. Raj, it says D5W, how can that be pure water? Listen, clinically, this is equal to pure water. Why don't you just give pure water, Dr. Raj? Because listen you got this. If you put pure water into your patient, oh! my goodness, the water is going to do what? It is going to equilibrate throughout the total body water. Really quick. What you are worried about when you put too much water strictly? It is going to go straight into the cell. What don't you just kill your patient? Just resign from your job. Leave now. Never practice medicine, please. Don't do that. So you are not going to infuse pure water. But say that you have a situation that you need to give hypertonic fluid, D5W. What is it going to do? Listen. This is dextrose 5 percent with water. What is dextrose? Think of it as being like glucose. Listen to this. You have done this in physio. 22:05 Let us do it now clinically. If you have glucose, at first if you infuse it and along with it attach to the water. So this is pretty much obligated water and you want to give hypertonic fluid for whatever reason in your patient. And so now you want to retard, you want to delay that water from entering the cell, don't you? D5W will help you do that. 22:35 D5W, the 5 percent dextrose is just enough in which it will delay the entry. Take a look of that water into the ICF so that you do not have swelling and bursting of your, you don't want fireworks in your plasma. Trust me. So you don't wan tto have excess swelling and D5W accomplishes that exact task. Now we have ICF contraction. This will be what kind of issue? Give me condition in which your volume from the ICF is being pulled out into the ECF. Take a look at hypernatremia or excess let us say glucose, uncontrolled diabetes mellitus.
About the Lecture
The lecture Extracellular Fluid (ECF) and Intracellular Fluid (ICF): Clinical Volume Dynamics by Carlo Raj, MD is from the course Fluid and Electrolyte Balance.
Included Quiz Questions
Which of the following scenarios would result in a decreased effective circulating volume with a normal extracellular fluid volume?
- Global vasodilation
- Protein wasting in the urine
- Water deprivation
- Inefficient cardiac pump
- Inability to produce albumin
When does a decrease in effective circulating volume equal the decrease in extracellular fluid volume?
- Loss of isotonic fluid
- Loss of free water
- Loss of hypertonic fluid
- Loss of salt
- Loss of protein
Which of the following scenarios would NOT result in an increase in extracellular fluid volume?
- Patient with sepsis
- Patient with cirrhosis
- Patient with Kwashiorkor
- Patient with nephrotic syndrome
- Patient with congestive heart failure
Which of the following changes would you expect to find in a patient with water deprivation?
- Increase in intracellular fluid osmolality
- Increase in extracellular fluid volume
- None are correct
- Increase in intracellular fluid volume
- Decrease in extracellular fluid osmolality
Which of the following patients is most likely to show an increase in extracellular fluid volume and no change to intracellular fluid volume or osmolality in either compartment?
- Patient with an infusion of isotonic saline
- Patient with an infusion of D5W
- Patient with diarrhea
- Patient with Addison’s disease
- Patient with syndrome of inappropriate antidiuretic hormone
What is the most important factor to consider when predicting fluid shifts between the intracellular fluid compartment and the extracellular fluid compartment?
- Extracellular fluid osmolality
- Extracellular fluid volume
- Effective circulating volume
- Intracellular fluid volume
- Patient characteristics
Which of the following scenarios would result in an increase in extracellular fluid volume and osmolality, with a decrease in intracellular fluid volume?
- High salt intake
- Infusion of isotonic saline
- SIADH
- Adrenal insufficiency
- Water deprivation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I find Dr .Raj to be energetic, fun and I appreciate him taking the time to teach us concepts and foundations as opposed to blindly memorizing facts. Enjoying his series thoroughly!
Brilliant! Dr. Raj focuses on understanding and establishes foundation knowledge for you to build on. Extremely helpful.