Playlist
Show Playlist
Hide Playlist
Asthma: Lower Airways Obstruction
-
Slides 03 Asthma RespiratoryAdvanced.pdf
-
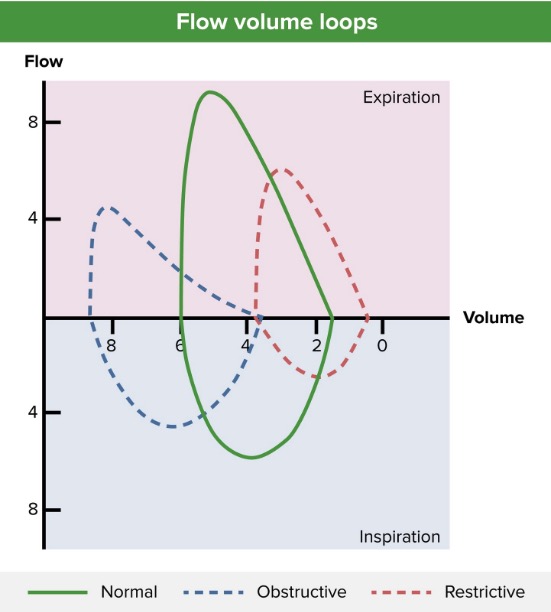
Download Lecture Overview
00:01 So the subject of this lecture is asthma, which is one of the common forms of airways disease that affects respiratory patients. When we talk about airways disease, we mean diseases that affect the conducting airways, the trachea, the major bronchi, and the bronchioles going down as far as the terminal bronchioles. We don’t mean diseases affecting the alveoli. 00:26 These airways diseases, in general, will present with some form of airways obstruction. 00:31 And that will be recordable when you do lung function test as obstructive lung function changes. 00:38 They don’t tend to show many abnormalities on a chest X-ray. That is because the bronchi are not readily detectable on X-ray, and the changes we’re talking about are relatively small changes in multiple different parts of the airways rather than a single mass lesion as if you have a cancer, for example. There are a range of potential airways diseases. 01:02 However, this subject is dominated by two airways disease; asthma and chronic obstructive pulmonary disease. COPD, this is a subject to the next lecture as really a smoking-related lung disease. In this lecture, I will concentrate largely on asthma. In addition, I will cover post-infective bronchial hyperactivity. At third lecture, we'll discuss other airways diseases, the causes of large airway obstruction, bronchiectasis, and allergic bronchopulmonary aspergillosis. A major thing about airways disease is that the obstruction that occurs can be described as reversible or irreversible. So the prevention of effective airflow can be reversed, in reversible disease, can be improved of treatment, whereas, with irreversible disease, it can’t be. That’s the broad distinction. 02:09 There are of course patients in between with partially reversible airways disease, where the obstruction can be partially reversed but doesn’t get as good as normal. 02:19 Largely speaking, asthma is a reversible airways disease, whereas, COPD is an irreversible airways disease. 02:28 Another important thing about airways disease is that expiration is always worse than inspiration with the lower airways obstruction problems. As a consequence, that means if you have significant lower airways obstruction, then you’ll end up with a degree of air trapping and accumulation of air in the lungs increasing the volume of the lungs, increasing the residual volume specifically, and making the lungs hyperexpanded. So, to talk about reversibility in a bit more detail as this is a fundamental concept for airways obstruction. What we mean by reversibility is that if there’s a 15% increase in your forced expiratory volume in one second, a measure of airflow on expiration, and that’s at least 200 ml, then there is a degree of reversibility present. Now, if that reversibility of treatment actually improves your FEV1 to the expected level for somebody of your age, sex, and height, then that will be a fully reversible situation. But if it only goes apart of the way to what you might expect to have as your FEV1, then that’s partially reversible. And that shown by this diagram on the right-hand side of this slide, the patient’s pre-treatment, pre-bronchodilator data, given FEV1 of 1.2. 03:51 Then the patient is given some salbutamol and the FEV1 increases by 700 ml, and by over 50% to 1.9. SO that's a substantial degree of reversibility. However, because of the age, sex, and height of this patient, the FEV1 is expected to be closer to three about 2, 2.8. And yet, they’ve only achieved 1.9 of the bronchodilation. So that’s a partially reversed situation. Now, reversibility in asthma is often clinically very obvious. The patient may come into hospital in exacerbation, be terribly breathless, and then two weeks later, be back running their five kilometers a day. So that clearly shows somebody who has an airways disease which can be very severe, they end up in hospital. But when they’re well, it can actually allow them to function at a very high level. The treatment that we use to test for reversibility is usually just some inhaled bronchodilator, a beta2 agonist such as salbutamol, and that can be inhaled using a normal inhaler or a nebulizer. Sometimes, when we really want to test whether somebody is reversible, we increase the power of the treatment by giving them oral prednisolone, corticosteroids for three weeks potentially, and potentially giving them a nebulised salbutamol over that time. That’s the real test for full reversibility in patients where it’s not clear that their lung function can return to normal with just taking an inhaled bronchodilator. Now, as I mentioned already, asthma is largely a reversible airways disease. And COPD is largely an irreversible airways disease. But there’s such a large range of types of asthma and COPD that there is an overlap. Some patients with COPD have degree of reversibility. And some patients with asthma, especially those patients who had the disease for a very long period of time or poorly controlled disease, will develop irreversible components as well. So there is an overlap between the two. 05:59 Another airways disease, for example, bronchiectasis, can also have reversible and irreversible and a partially reversible patients with the airways obstruction. And there are less common causes of airways obstruction, which, in general, tend to cause largely irreversible airways disease. And I’ll talk about those a little in the second lecture. So, it’s quite easy to get confused between reversible and irreversible airways disease in asthma and COPD. But the basic concept is relatively straightforward. Reversibility indicates asthma. Irreversibility suggests COPD, but there’s more to that. Patients with COPD need to have a smoking history. But there are patients who do overlap in the middle. For example, if you have an asthmatic who’s been asthmatic since childhood but has been smoking since the age of 20, at the time they get to 50, actually, they may acquire a significant degree of airways obstruction which is irreversible, and that would be COPD because of the smoking on the background of asthma. So, asthma is the commonest chronic
About the Lecture
The lecture Asthma: Lower Airways Obstruction by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Airway Diseases.
Included Quiz Questions
Which of the following changes in lung function testing results is seen in lower airway obstructive processes?
- Reduced FEV1 with a ratio of FEV1 / FVC less than 70%
- Reduced FEV1 and FVC with a ratio of FEV1 / FVC greater than 80%
- Reduced FEV1 with an increased FVC
- Increased FEV1 with a reduced FVC
Which of the following diseases can obstruct the large airways?
- Malignant lesions
- Allergic bronchopulmonary aspergillosis
- Asthma
- COPD
- Cystic fibrosis
Which of the following lung volumes will increase significantly when air trapping occurs in the lungs of patients with asthma?
- Residual volume
- Inspiratory reserve volume
- Expiratory reserve volume
- Tidal volume
- Vital capacity
Which of the following is NOT part of the clinical definition of reversible asthma?
- Increase in the residual volume by 100 ml after bronchodilator administration
- Increase in FEV1 by more than 200 ml (> 15%) after bronchodilator administration
- Major changes in PEFR over time
- Clinically obvious reversibility
Which of the following is the treatment for simple reversible asthma?
- Inhaled short-acting beta agonists
- Oral corticosteroids
- Inhaled ipratropium bromide
- Intramuscular epinephrine
- Oral propranolol
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
4 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great content, well-explained and the lecture was easy to follow. Thanks!
Good lecture. Well explained and with good illustration without much of text info in slides
Very well Explained, Very good faculty. All the required stuff in the lecture.
I really liked this lecture a lot and I wanted to say it because of a rude coment that I saw on the comment section