Playlist
Show Playlist
Hide Playlist
Diabetes Insipidus (DI): Overview
-
Slides DiabetesInsipidus RenalPathology.pdf
-
Download Lecture Overview
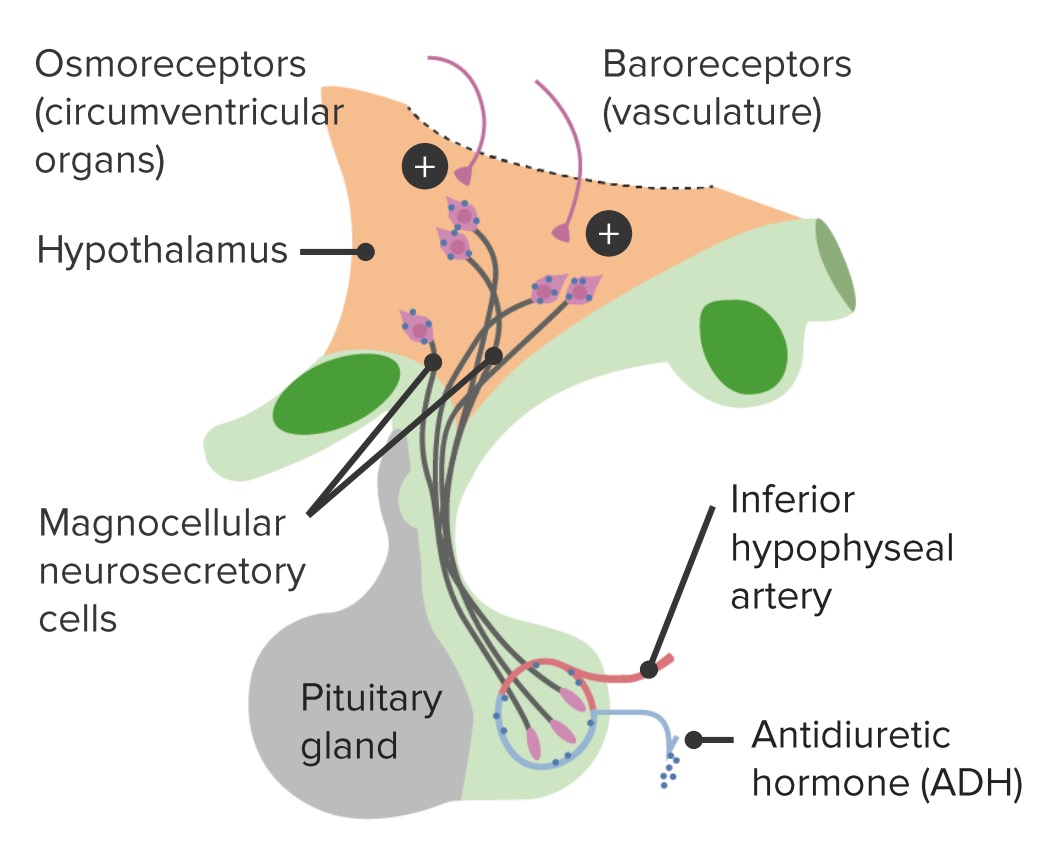
00:01 Continuing our discussion on the concentration of urine. Up until now, we looked at ADH, looked at its control and then went into SIADH in great detail. Now let us take a look at diabetes insipidus, the opposite of but nonetheless an important difference to keep in mind when you have plasma and urine osmolarity at hand. So we have nephrogenic diabetic insipidus. 00:26 Now what we will do here ladies and gentleman is under renal or nephrology, we will strictly only be managing nephrogenic diabetic insipidus. I want to make sure that we are clear because there is no important piece of information that is left out in your lecture series with me. The central diabetes insipidus, we will be dealing with that in endocrinology. Is that clear? So here let us keep things relevant and all that I will bring to your attention is the pathology of diabetes insipidus, nephrogenic in the category of nephrology. With that said, let us continue and before we move on, though, let us talk about the basic definition and predict as to what is going to happen in our patient with nephrogenic diabetes insipidus. 01:13 Nephrogenic that means there is a problem with the kidney in which ADH is not working properly. Now just to make sure we are clear. If you have a patient that has SIADH maybe perhaps secondary to small cell lung cancer. We talked about that in great detail. Then you would purposely induce nephrogenic diabetes insipidus by giving a drug such as demeclocycline so that you can deal with SIADH. However now we will come to the actual primary disease of nephrogenic diabetes insipidus. There is not going to be your V2 receptors working properly. You are not going to be able to properly reabsorb your water. If that is the case, you are going to create massive diluted urine. This clearance of that water, which is free will be absolutely positive. Remember the clearance of water is zero and that is where all are really focused upon if clearance of water was zero. It is the fact that you are producing urine that is obligated meaning with sodium. It is not free of solute, but if you are producing lots of diluted urine and you are clearing this and understand there is going to be a lot more free water than there is going to accompanied with solute. 02:34 So there is going to be a lot more free water thus the clearance of water here is going to be positive. All that is what we predicted. Let us continue. 02:45 Plasma osmolarity increase. Are you seeing it? You are losing diluted urine thus plasma osmolarity increases. It stimulates the posterior pituitary to do what? To produce even more ADH, but obviously, it is not going to do anything. So this is a condition in which and let us now draw some parallels. If the receptors are not working, give me some pathologies in which the receptors are not working properly. PTH receptors aren't working properly. What is that diagnosis? That is pseudohypoparathyroidism. Your testosterone receptors are not working properly. Give me that diagnosis. Androgen insensitivity syndrome. Your insulin receptors are not working properly. Give me that diagnosis. Diabetes mellitus type II. Here we have the receptors for ADH not working properly. Why am I bringing all this up? Technically speaking clinically. Each one of those situations that I just gave you including this one where we have ADH receptors and B2 receptors are not working. The PTH receptors in pseudohypoparathyroidism is not working. The receptors of testosterone is not working. The insulin receptor is not working. Clinically at some point in time in that disease course of those differentials that I gave you, you would always expect that whole amount level to be what? High, because the receptor is not working you are going to get feedback mechanism where all my goodness I want, I want, I want, I want more hormone, want more hormone, want more hormone, want more hormone. Hence in pseudohypoparathyroidism, you will find increased PTH. Hence an androgen insensitivity syndrome, you find an increase in testosterone. Listen. You could in diabetes type II within obese patient with insulin resistance actually have increased in insulin and you will. Hence, you will have many of the pathologic courses or sequelae that we see in diabetes type II. Here we are going to have too much ADH. Are you drawing the parallels now? I cannot talk about this in good faith without telling you that there are other diseases that have behaved the same way. Let us continue. So circulating ADH levels now you can see confidently and understand as to why it is elevated, but who is not responding? The principal cells. 05:11 Let us take a look at etiology of nephrogenic diabetes insipidus. The most common causes
About the Lecture
The lecture Diabetes Insipidus (DI): Overview by Carlo Raj, MD is from the course (Nephrogenic) Diabetes Insipidus (DI).
Included Quiz Questions
Which of the following conditions is not caused by defective receptors?
- Type 1 diabetes
- Type 2 diabetes
- Androgen insensitivity syndrome
- Pseudohypoparathyroidism
Which of the following parameters would be decreased in a patient with nephrogenic diabetes insipidus?
- Urine osmolarity
- Urine volume
- Clearance of water
- Plasma ADH concentration
- Plasma osmolarity
Which of the following statements is incorrect regarding nephrogenic diabetes insipidus?
- ADH release is inhibited from the posterior pituitary.
- Urine osmolarity is decreased.
- ADH receptors are defective in the principal cells.
- Plasma osmolarity is increased.
- Water reabsorption is decreased in the distal tubules.
Which of the following best describes the defect in nephrogenic diabetes insipidus?
- A defect in the receptors.
- Insufficient production of hormone.
- Excessive positive feedback.
- Insufficient precursors for hormone production.
- Autoantibodies
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |