Playlist
Show Playlist
Hide Playlist
Heart Failure (HF): Diagnosis and Treatment
-
Slides CongestiveHeartFailure CardiovascularPathology.pdf
-
Download Lecture Overview
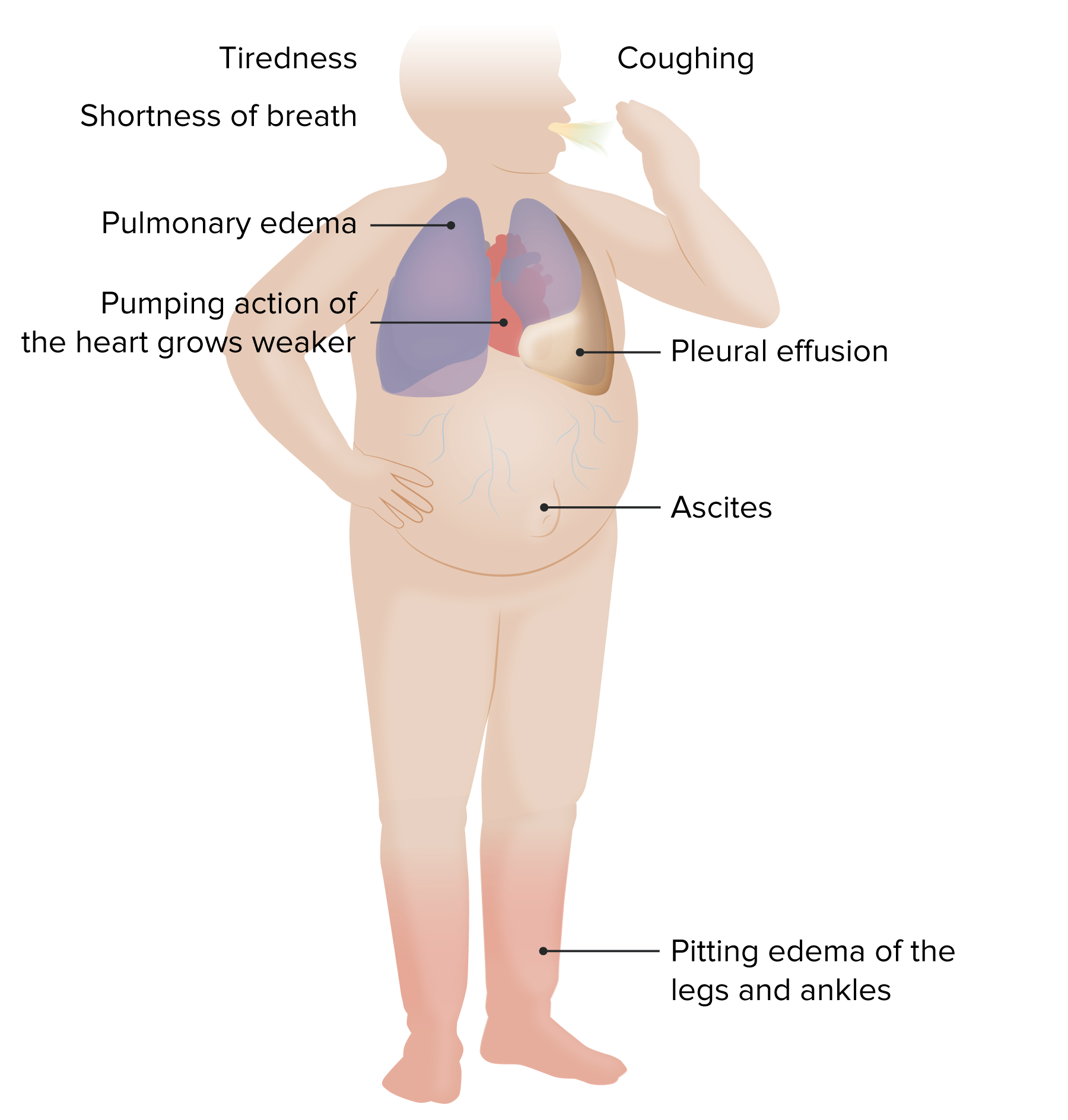
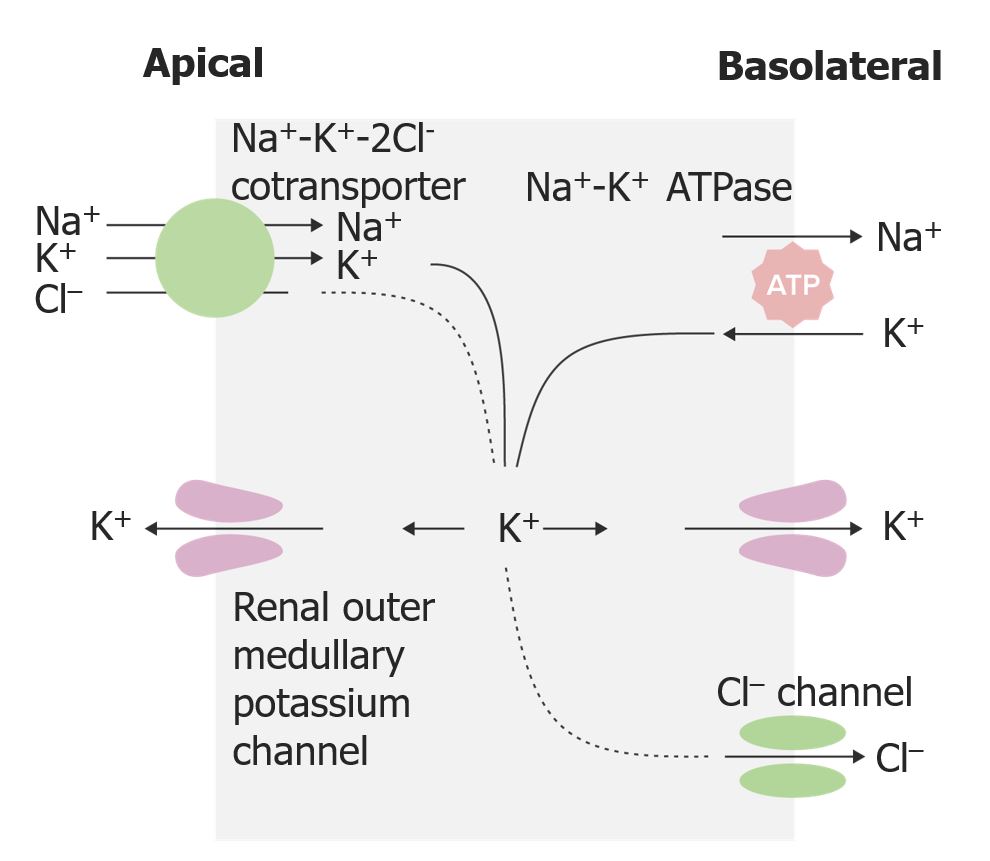
00:00 Physical examination. Left sided everything is pulmonary. Crackles. 00:07 Where? On both sides bilateral. What are you going to find on X-ray? You are going to find pulmonary edema and you will find opacity, both sides. Bibasilar crackles, bibasilar opacities because that is what edema looks like. What is this edema? It is transudate. 00:22 It is protein poor. Increased hydrostatic pressure that causes pulmonary edema, you tell me. Cardiogenic or noncardiogenic cause the pulmonary edema? Obviously cardiogenic, is that clear? Transudate. Increased hydrostatic pressure. Obviously, there is a reason as to why I asked you that question because later on we will talk about noncardiogenic type of pulmonary edema in pulmonology. And when we do so, then we will refer to what is known as increased capillary permeability. Therefore, there would be exudate and protein rich. Now it is transudate. S3 gallop, what does that mean to you? CHF, large left ventricle. Blood is gushing into left ventricle in a hurry and you are going to create an S3. 01:06 Where? After S2. Come on bring these stuff together. You got this or you? You have control of your education? Doesn't that feel good? Right-sided heart failure. Positive JVD, pitting lower edema. What does pitting mean to you? Transudate. Protein poor. 01:28 Perhaps ascites and hepatojugular reflux. What does that mean? A touch upon the liver upon inspiration comes a jugular. Not good. Right-sided heart failure. Ask you a question. It is typical question, which you can do this. Cor pulmonale. No that is not what this is. Right-sided heart failure secondary to left-sided heart failure is a particular topic here. I will just make sure we're clear. At some point we'll go into cor pulmonale and then I will start talking about pulmonary fibrosis, talk about pneumonia, lobar type of consolidation so on and so forth. At this juncture, not yet. Chest X-ray, well here you have a large apex, cardiomegaly. Talked about this a number of times. Now the curly B lines represent? Well tell me about lymphatics? When it rains, on the roads, well you have the gutter system, which is responsible for removing that excess fluid. That is with the lymphatics or the lymphatics are the gutter system of the roads. The lymphatics are responsible for, in the interstitium to remove the excess fluid. How can you confirm this? What if your patient had lymphoma? What if your patient had a tropical disease such as elephantiasis secondary to which area of Bancroft? What is that going to do? Block off the lymph. When you block off the lymph, my goodness you cannot drain out the fluid. What do we call that? Lymphedema right. So my point is this. When you have excess pulmonary edema obviously the lymphatics are quite active. Welcome to Kerley B lines. The echo, what do you going to find? A systolic ejection fraction that is decreased. Clear? What do you want to do with this patient? Management. 03:09 Overall, improve quality of life, increase comfort. How do you do that or maybe something as simple as recommendation? A couple of pillows. At all cost, you want to try to reduce the amount of time this patient spends in the hospital. Absolutely. Prolonged life, treat with proven therapies that is going to do what? Decreased mortality. What does that bring us to? Neurohormonal blockade. What kind of drugs are you thinking about? How about spironolactone? How about ARBs? How about ACE? Really. Spirinolactone what does that knocking out? It is an aldosterone receptor antagonist. You are not using it for its potassium sparing effect or quality. That is great, but really that is not te point. It is the fact that you are knocking out all those. What does remodeling mean by the way? Remodeling is the fact that the heart is trying to regenerate, but the problem is it might then actually introduce fibrosis. And when you do so during the repair process, you might then actually end up creating more harm than good. And if you are able to slow down or perhaps even inhibits some of that remodeling, then just may be you might be able to increase the survival time of your patient. Wonderful. You look for those type of drugs. Neurohormononal, by that beta-blockers, metoprolol. ACE inhibitors, you don't produce aldosterone. You have ARBs. You block your aldosterone. Aldosterone receptor antagonist. 04:39 Welcome to spironolactone. Is that clear? Correct underlying cause absolutely. May be this congestive heart failure was due to some kind of valvular defect. Aortic stenosis, mitral regurgitation. Revascularization if needed. So, for example, if this particular CHF was caused by MI, why not try to go in there and do percutaneous type of intervention, PCI, coronary artery bypass grafting if needed. Treat hypertension, thyroid disease, autoimmune all of the different causes of heart failure that we have covered in this lecture series. 05:17 Stop offending medications. May be calcium channel blockers and maybe perhaps NSAIDs. 05:23 Quality of life. Sodium, cut it down. May be loop diuretic to improve, get rid of the pulmonary edema. "I have a hard time breathing doc!" Alright let's get rid of some of that fluid. Maybe you feel a little bit better. Obviously you are not treating the congestive heart failure. You are treating the symptoms for the patient. What is a symptom? The patient is expressing trouble. 05:45 What is sign? You as a clinician finding the edema. Think PT and symptom that your patient is expressing. The sign is you. You are the sign. That is then going to find the different clinical manifestations of a disease. Reduce hospitalization. How are you going to go by doing this? Maybe perhaps positive inotropic agent if needed. What does it do? It blocks the sodium-potassium ATPase pump on the basolateral membrane. So therefore where is my sodium? You tell me. You got this. Sodium is accumulating where? Inside my myocardiocyte. If it is accumulating within my myocardiocyte, it is not being pumped out and so, therefore, no sodium is coming in and calcium is not leaving. So indirectly what are you doing? You increase your intracellular amount of calcium. And that intracellular calcium that you are increasing is then going to perhaps bind to your troponin C or maybe perhaps even increase the amount of calcium that is being released from the sarcoplasmic reticulum. You see as to how everything is being integrated. You see as to how by learning your basics and you find in getting digoxin digitalis and such that by increasing calcium, then you might do what? You might be increasing your positive inotropic affect. 06:58 Fantastic. Now the part that you want to worry about is well there is every possibility afib kicking in. So that you want to be careful for a number of reasons. Now, treatments for neurohormonal. Well what do you want to do here? You want to try to decrease the afterload. You can do so by giving angiotensin type of inhibitors and so, therefore, the less amount of angiotensin II, then you have less vasoconstriction. You decrease your afterload. Does that help with cardiac output? Yeah. Does that ACE inhibitor also increases quality of life because it inhibits remodeling? The classes of medications which are currently included in guideline-directed medical therapy and have been shown to reduce morbidity and mortality in patients with heart failure include the following: ACE inhibitors, angiotensin receptor blockers, or more recently, the angiotensin receptor-neprilysin inhibitor sacubitril-valsartan; beta blockers (such as metoprolol); sodium-glucose cotransporter 2 inhibitors (which can be used regardless of whether the patient has diabetes); and mineralocorticoid receptor antagonists, such as spironolactone. 08:04 Look for these. All depends as to what that question is, what your attending is going for. Are you trying to treat the pulmonary edema? Please don't say ACE inhibitor there. You will be a left out of your rotation. Pulmonary edema, furosemide. Get rid of your fluid. If you want to improve the quality of life, then you start thinking about these drugs. Is that clear? Yes.
About the Lecture
The lecture Heart Failure (HF): Diagnosis and Treatment by Carlo Raj, MD is from the course Heart Failure: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following statements about edema in the setting of congestive heart failure is FALSE?
- The fluid in pitting edema is exudative.
- The fluid in pitting edema is a transudate.
- Right-sided heart failure is associated with jugular venous distention.
- Left-sided heart failure leads to pulmonary edema.
- Edema is the result of increased hydrostatic pressure.
What is the mechanism of action of digoxin?
- Inhibits Na+/K+ ATPase pump in myocardial cells
- Inhibits Ca²⁺ channels
- Inhibits AT-II receptors
- Stimulates alpha-2 adrenergic receptors
- Inhibits beta-1 receptors
Which of the following medication classes does NOT reduce mortality in patients with congestive heart failure?
- Calcium channel blockers
- Beta blockers
- ACE inhibitors
- Nitrates
- Angiotensin receptor blockers
What is the primary driving force in the formation of transudative edema?
- Increased hydrostatic pressure
- Decreased hydrostatic pressure
- Increased oncotic pressure
- Decreased oncotic pressure
- No known effect
What is the usual abnormal heart sound observed in left-sided heart failure?
- S3 gallop
- S4 gallop
- Systolic murmur
- Holosystolic murmur
- Diastolic murmur
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |