Playlist
Show Playlist
Hide Playlist
Auscultation Areas
-
Slides Heart Sounds Cardiovascular Pathology.pdf
-
Download Lecture Overview
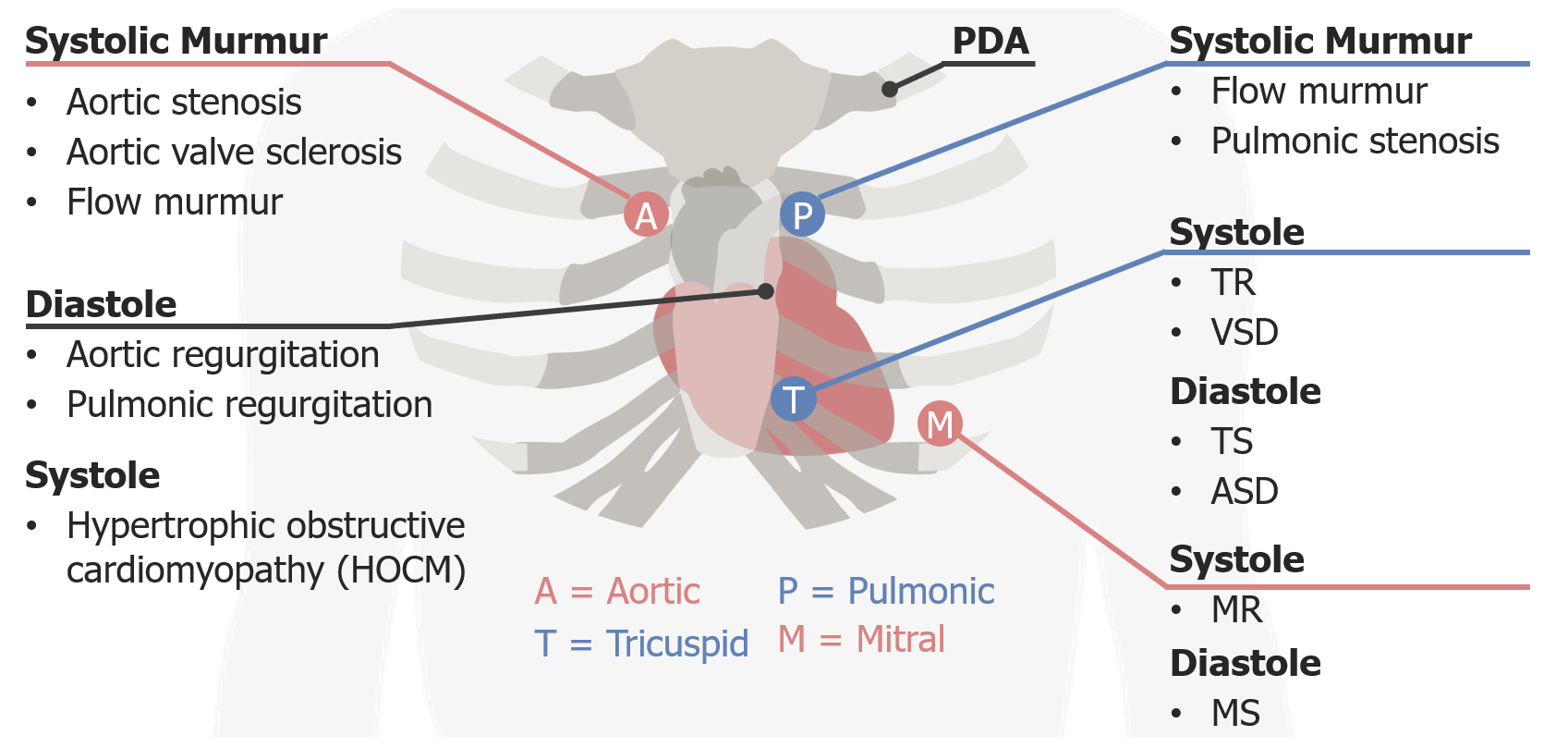
00:00 Let us take a look at our chest and how important is this? Really important. So take a deep breath. Stick with me and I am going to walk you through this. Alright, now as we go through this, I would like for you to point to your own chest where we are. By looking at this, well remember a mirror image. So we have aorta. The aortic valve would be right parasternal second intercostal space. Are you pointing to it? That is where it is, why? Do this for me. Here is your left ventricle and you have your aortic arch, anatomy. So where is my aortic valve? Right second intercostal space. What about the pulmonic valve? Second intercostal space, left parasternal. Where is your right ventricle? Down by the parasternal on the left side and so, therefore, pulmonic valve will be here. Are we clear? That is normal. 00:48 We are not doing any pathology right now. I want you to go into the fourth intercosal space now. We are still on the right side of the heart. Picture that, conceptualize that for me. Good. And fourth intercostal space left parasternal, that's your tricuspid, T. Then we have our mitral. All these you talked about in anatomy, physio. Now we are going to put these together and put some pathology studies. Your mitral is going to be where please? Apex. Where is your apex located in normal heart? Fifth intercostal space, midclavicular, right about here. How many times have we talked about midaxillary? A few times. There will be a lateral displacement. Automatically gives you what? You are thinking about cardiomegaly or whatever reason. But fifth intercostal space midclavicular is your mitral. Alright, normal. 01:36 Let us put in some pathologies. So begin with the systolic murmur here, right aortic side. 01:42 With an aortic side, who is your patient? I'm just going to give you one little clue clinically for each one of these major murmurs and then we will get into these in greater detail as we get into valvular pathology. Okay. Not to worry. 01:54 Aortic stenosis. "Hey doc, 32-year-old and feeling tired at walking a few blocks, may or may not have chest pain. When I walk with my dog and after a few blocks, I feel tired and I feel little dizzy, chest pain. But then I stopped and it goes away." Or the patient may not have chest pain. But does he feel fatigue? Maybe a little bit of dizziness. Next, upon cardiac auscultation, you hear a murmur second intercostal space right parasternal and you hear the murmur radiating up into carotid. Diagnosis, right off the bat, aortic stenosis. Tell me about this patient. Wow! Walking the dog felt tired, maybe perhaps chest pain maybe not. What is all that about? If you have aortic stenosis, tell me about stenosis, rigid aortic valve. It doesn't want to open. So what happen to cardiac output? We have decreased cardiac output. How are you going to feel? Not too great. You may find a little tired or maybe perhaps there might be angina. We will talk about this and tell me about the murmur. Where was it radiating to? Radiating up into the carotid. Not the blood. Your patient wasn't doing this. Yes sir. The patient wasn't doing that. That's aortic regurg. 03:11 We will come to that later okay. Right now, aortic stenosis. Don’t worry all I am doing is introduction. You expect to hear that where? Right second intercostal. What about some of these others? Aortic valve sclerosis as the differential and a flow murmur with increased amount of blood passing through there. 03:26 Let us move on to another one. Another area here would be your pulmonic area. Where am I? Second intercostal left parasternal. Here you might be thinking about pulmonic stenosis. Differential? Maybe something like tetralogy of Fallot, pulmonic stenosis or maybe it was an infection. Really? What kind? Tell me a virus that may result in pulmonic stenosis. You're telling me. Rubella. Let's continue, and then we have in the tricuspid area, we are going to divide this as and you want to do the same please so that you keep your thoughts organized, systolic and diastolic, and I want to walk through the easy one first. 04:05 Let us do systolic first. First where am I? Fifth intercostal and left parasternal. Stick with me. Lot of information, this will be repetitious and I will keep reinforcing it but it begins with understanding where you are as integrate. That is the name of the game. So here let us begin with tricuspid regurg. How do that occur? Maybe it is due to an IV drug abuser or maybe there was issues with the carcinoid. Okay anyhow, you are on the right side of the heart, left parasternal fifth intercostal and it is a systolic murmur. What does that mean to you? That means that the tricuspid valve does not want to close. Which way does it normally close? The tricuspid valve, here is my right ventricle and here is my tricuspid valve and here is my right atrium. And the valve was supposed to close this way, but it does not close properly and it just opens up during systole. What does that mean to you in terms of your murmur? Between S1 and S2, you can hear all the systolic murmur. 05:04 We will be spending time with that. Not to worry. Where am I? Left parasternal fifth intercostal. 05:11 VSD, very common. One of the most common congenital heart diseases is the ventricular septal defect and that will be a systolic murmur. What kind of shunt is this please? It is a left to right shunt. "But Dr. Raj, why did you say in tetralogy of Fallot, that there is a right to left shunt when that patient had a ventricular septal defect?" In tetralogy of Fallot, did you have a VSD? Yes, you do. Why is there a right to left shunting and here you're telling me it is left to right? Because, in tetralogy of Fallot, you had number 1 pulmonic stenosis resulted in right ventricular hypertrophy. You did have a VSD and the blood was rushing from the right ventricle into left ventricle. There is a right to left shunt. Here it is a left to right shunt. 05:54 This is not tetralogy. I am just strictly saying VSD. Well with diastolic murmur, a tricuspid stenosis. 06:03 The most common cause of tricuspid stenosis is rheumatic heart disease, while tricuspid regurgitation may be related to endocarditis associated with I.V. 06:10 drug use. 06:11 but it is not. So, therefore, if you hear a diastolic murmur after S2 and you are at the fifth intercostal space, left parasternal, welcome to tricuspid stenosis. Okay. Now let us integrate atrial septal defect. We are going to have fun here. Ready? Atrial septal defect. 06:25 What heart sound are you paying attention to? S2. With S2, what kind of split is this? A physiologic splt, a widened split or a fixed split? You tell me. Fixed split. Blood was always rushing from your left atrium into right atrium and, therefore, S2, A2, P2 was always fixed between your inspiration, expiration. It didn't change. But that is a fixed split. How can you then bring this into a diastolic murmur? Listen. So now the blood is rushing into where? Into the right atrium. Fantastic. When is the tricuspid valve supposed to open? During systole or diastole? Diastole. What is the definition of a murmur? Increased turbulence across a valve. With all this blood in the right atrium and passing across a tricuspid valve, are you not increasing your turbulence? Of course, you are. Could you result in a diastolic murmur at the fifth intercostal space, left parasternal? Are you pointing to it? Please do it now. 07:35 At the atrial septal defect, now clinically you can go one step further, that mean to say that eventually you might find issues up by the pulmonic area as well. That must be understood. 07:45 But go step by step, builds upon a foundation so that you never crumble. If your foundation is never strong like a building, what is going to happen? Have a tornado. What have you and then the building is gone. Because the foundation was weak. Your foundation is strong, no matter what they throw at you, the attending, licensing board, you are guaranteed to get that question right because your foundation is solid. And that's what we're going to build here together. Let's continue. And finally, we have our mitral area. Where are you? Fifth intercostal space and you're at the midclavicular. Pretty straightforward, but these will be a mitral valvular issues and we will get into greater detail. You all know about mitral regurg, take your time. The mitral valve is supposed to close from the left ventricle towards left atrium and if it doesn't close properly, you have a holosystolic murmur between S1 and S2, don't you? And where would you hear this? By the fifth intercostal space and by the midclavicular or mitral stenosis. If you have mitral stenosis, let's say chronic rheumatic heart disease. Chronic rheumatic heart disease may result in mitral stenosis. The mitral valve doesn't want to open, even opening snap, it's a middiastolic murmur and then you have this particular murmur taking place at the same location. Fifth intercostal space, midclavicular. 09:03 I sound like a broken record but it is okay. Keeps saying this over and over again so my voice haunts you whenever you might be posed with the question. 09:12 And then finally we have PDA, patent ductus arteriosus. What happened here? The ductus arteriosus is sitting closed and so, therefore, close your eyes. Tell me about this ductus arteriosus. What are you connecting? You are connecting the aorta to the pulmonary artery. You with me? The aorta with the pulmonary artery is what you are connecting. And upon birth, you have the ductus arteriosus still open, then where is this blood going? The blood is going from the aorta into the pulmonary artery because you should know the systemic pressure is quite high when compared to pulmonic. 09:46 So, therefore, what kind of murmur you are going to have. What did I just do? That is a machine murmur and at no point with my particular rendition. Let us make an album called "Dr. Raj's valvular heart sounds". At no point in my rendition of your PDA, could you differentiate between S1 and S2, could you? You couldn't. Welcome to PDA. We will be spending time, not to worry, with the pathophys of every single one in the valvular heart diseases and the question that you might get would be one in which you go on and there is the computer. You have to put on headphones. You listen to the heart sounds and they will ask you and they'll put a chest on your screen. A, B, C, D, E so forth and then they will ask you, well where exactly on this chest would you expect to heart this particular valvular heart sound? Last few points here with our location of a couple of important valvular heart diseases and it could be a little tricky if you are not paying attention so I really want you to look at me and pay attention to what I am saying. First and foremost, we are on the left parasternal, approximate the third intercostal space, that would be the best location. Let us talk about the first one. This patient here is the one that would be perhaps presenting with yes sir. Head bobbing. I feel my radial pulse in it, wow I can really feel it. It's bounding. 11:14 It is a bounding pulse. Aortic regurg is what we're referring to. Now if there is aortic regurg, give me some differentials of aortic regurg. Maybe consgestive heart failure. Aortic root is becoming dilated. Maybe this patient has ankylosing spondylitis. Look at me. I am pretty stiff as this, but when I bend over, my back and my vertebrae have a proper curvature. 11:37 Okay if I was half my age and I was 20, I just give way my age whatever. So if I was 20 and I was bending over and I didn't have a proper curvature my vertebrae, what is my diagnosis most likely? Ankylosing spondylitis. Why am I bringing this up? Because with ankylosing spondylitis what might be its associated valvular heart disease? Aortic regurg. Do not forget that. Please ever. My point is this. 12:04 Now I want you to think about that anatomy again, of the aorta. So we have left ventricle, aorta. 12:09 If you have regurg, then blood is rushing from the aorta, back into the left ventricle, is it not? Of course it is. And this is occurring when? During diastole, isn't it? Because during diastole is the one that aortic valve should close. Don’t worry we will go through all this again, but I am just putting all this together for you because this is how good you need to be. So now you have after S2, early diastolic murmur moving towards the apex so, therefore, aortic regurg would be expected to be heard best at the third intercostal space, left parasternal. So what kind of question might you get? While you walk in and you have your headphones and they give you a chest on the screen and the chest on the screen will have A, B, C, D, E. And then you'll have to listen to the heart sound and then you would have to locate where exactly on the chest you would hear aortic regurg in this or where it would be? A diastolic. Now if it was pulmonic regurg, pretty straightforward. 13:04 Pulmonic regurg, you had the second intercostal space left parasternal and you are going to regurg back into right ventricle so that you would expect to hear it around here as well. 13:15 Third intercostal space, left parasternal. Then we have this patient. If this was a young patient, not obese, no rheumatic heart disease, no bicuspid aortic valve, none of those issues, but was an athlete. Maybe a volley ball player, maybe a tennis player and when they are going for their volley either for the ball, well they fall. And when they fall, they will never get back again. They will never get back up, sudden death. That is sad. This then brings us to an unfortunate pathology called hypertrophic obstructive cardiomyopathy. What does that mean? What obstructed the outflow tract of what? Close your eyes. What's obstructed is the outflow tract from the left ventricle towards the aorta. You with me? So, therefore, where would you expect to hear this murmur, the systolic murmur when the blood is trying to be ejected? Once again third intercostal space approximally left peristernal. Hope that is clear.
About the Lecture
The lecture Auscultation Areas by Carlo Raj, MD is from the course Heart Sounds.
Included Quiz Questions
What valvular disease is associated with a crescendo-decrescendo systolic murmur at the right upper sternal border that radiates to the carotids?
- Aortic stenosis
- Aortic regurgitation
- Mitral stenosis
- Mitral regurgitation
- Hypertrophic obstructive cardiomyopathy
Which of the following murmurs may be heard with pulmonic stenosis related to rubella infection?
- A systolic murmur that increases with inspiration, best heard at the 2ⁿᵈ intercostal space, left parasternal border
- A systolic murmur that decreases with inspiration, best heard at the 2ⁿᵈ intercostal space, right parasternal border
- A diastolic murmur that increases with inspiration, best heard at the 2ⁿᵈ intercostal space, left parasternal border
- A systolic murmur heard throughout the precordium
- A diastolic murmur heard throughout the precordium
Head-bobbing and a bounding pulse are characteristic for what valvular heart condition?
- Aortic regurgitation
- Aortic stenosis
- Tricuspid regurgitation
- Mitral stenosis
- Ventricular septal defect
With which of the following conditions does the heart murmur increase in intensity on standing?
- Hypertrophic obstructive cardiomyopathy
- Atrial septal defect
- Mitral regurgitation
- Pulmonic stenosis
- Aortic regurgitation
Which of the following conditions presents with a continuous "machinery" murmur?
- Patent ductus arteriosus
- Pulmonary stenosis
- Atrial septal defect
- Ventricular septal defect
- Aortic regurgitation
What valvular condition causes an isolated diastolic murmur that increases on inspiration and is best heard at the 5th intercostal space on the left parasternal border?
- Tricuspid stenosis
- Aortic root dilation
- Aortic sclerosis
- Congenital infection with the rubella virus
- Patent ductus arteriosus
Which description best describes the murmur of aortic regurgitation?
- Diastolic murmur heard best at the left parasternal 3rd intercostal space
- Diastolic murmur heard best at the right upper sternal border
- Systolic murmur heard best at the right upper sternal border
- Systolic murmur heard best at the left parasternal 3rd intercostal space
- Diastolic murmur heard best at the apex of the heart
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |