Playlist
Show Playlist
Hide Playlist
Acute Coronary Syndrome
-
Slides IschemicHeartDisease CardiovascularPathology.pdf
-
Download Lecture Overview
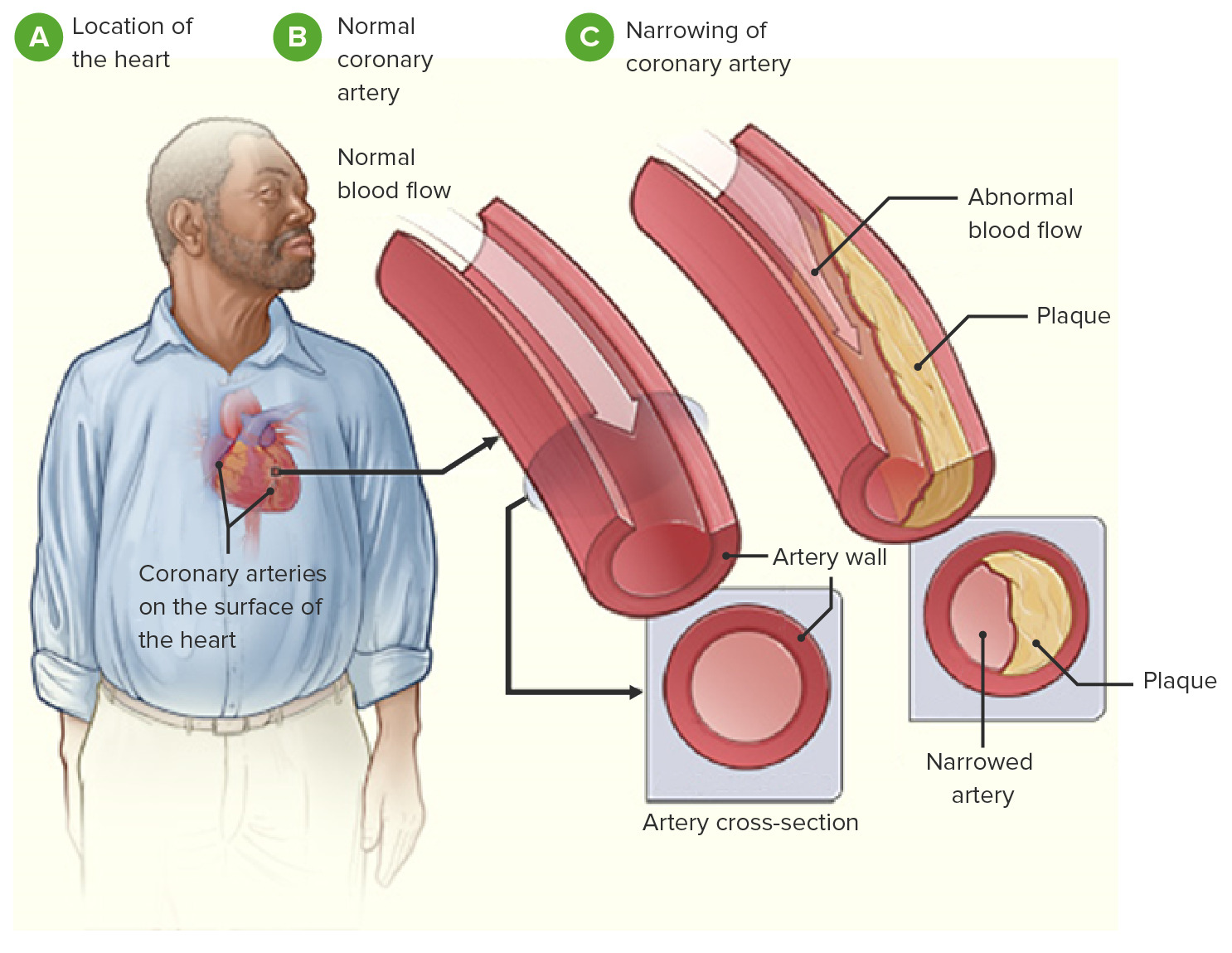
00:01 Continue our discussion of ischemic heart diseases. 00:04 Now, we take a look at acute coronary syndrome. 00:06 What's that mean to you? It means that we are one step closer having a myocardial infarction but not completely. 00:12 Acute coronary syndrome, we understand that our patient has a pain and may occur at rest. 00:21 Before we get in to any and all of this, just make sure that we understand some simple basic anatomy because as we get to the tail end of our lecture series, I'll have you take a look at EKGs, so that you know clearly the difference between what's known as a STEMI, an ST-Elevation Myocardial Infarction versus a non-STEMI. 00:40 Now before we get to any of that, then we're gonna build and build and build our pathology and our understanding so that you'll be able to clearly see this. 00:47 Now first, we have the aorta but then we have the left coronary artery. 00:51 Off the left coronary artery, that which is moving down between the ventricle. 00:58 It would be a left anterior descending as you should know from anatomy. 01:01 The left anterior descending, if it underwent major massive atherosclerosis and had an area in which there was a myocardial infarction. 01:12 Well, do you have any idea as to what leads every EKG that you might be paying attention to? That's important for you to understand and we will when the time is right, but just to give you an idea, if it's the anterior two-thirds of the interventricular septum that the left anterior descending is supplying and it's also supplying the lateral aspect of the heart a little bit, then what you might be thinking about? Well, the interventricular septum, you're still thinking about things like V1 and V2 leads, does that make sense to you? Then, as you move towards the apex of the heart, then you start thinking about V3 and V4, aren't you? I'm hoping that you have a pretty good idea as to what the leads of an EKG is going to be representing on the heart. 02:01 If you don't, that's quite alright because we'll be paying attention to this as we move further. 02:05 Now, acute coronary syndrome is what's you're seeing here as a bracket. 02:13 Before we get into acute coronary syndrome which should be a combination of unstable angina and acute MI, and I cannot have you memorize this, it's a build-up of atherosclerosis. 02:25 Let's go back to the concept of supply and demand, remember that? With supply, what then happened? The coronary arteries underwent occlusion and there was a progressive occlusion that was taking place that eventually resulted in pain in the chest even at rest. 02:45 And what about before that? Well, before that, it was stable angina and you keep this out of the discussion of acute coronary syndrome. 02:54 We take a look at stable angina, who's your patient? Coronary arterial disease, atherosclerosis, head to toe. 03:00 Remember we talked about this with cardiovascular disease including peripheral vascular disease, cerebrovascular accident, and our topic at hand which is coronary arterial disease. 03:11 Under stable angina, the precordial chest pain is exacerbated by either stress or exercise. 03:20 Now, by stress, there are a couple of ways that we can induce this, can't we? What's that mean? Well, your patient, let's say, is a 67-year-old female. 03:29 She tells, "Hey doc. I'm having chest pain when I'm walking a few blocks or when I'm walking up the stairs. 03:35 When I stop, the chest pain goes away." You do an EKG at rest, what happens? Everything comes back to normal. You say, "Bye-bye. Have a nice day." No, my goodness. 03:49 You want to stay in practice, right? Therefore, you have to then induce a stress test. 03:54 Now, if your patient has arthritis and the debilitating, please don't be a masochist and put your patient on a treadmill. 04:02 That's not very nice. Be nice to your patient. 04:05 We will get into what's known as your chemical stress test because that is incredibly important, but what kind of changes do you expect to see in EKG when you induce a stress? We'll talk about that coming up. 04:19 Now, once this patient is giving you such a history, what would you want to give that patient automatically? You give this patient something in which there's going to be relief from the chest pain, correct? What's that mean to you? It means underneath the tongue, anytime that there's chest pain, you place nitroglycerin, correct? Sublingual. When you place sublingual and it then dissolves and enters your circulation, what is it going to do your veins? Good. Vasodilate. When you vasodilate your veins, what does that affect? Preload or afterload, please? Good. Preload. You're going to decrease preload, and so therefore, you're going to decrease demand, aren't you? Of the heart, for oxygen, it's exactly what you're going for. Then, what about afterload? Well, it also causes arteriolar vasodilation. When you have arteriolar vasodilation, you're going to decrease TPR. 05:16 Let's move on. Now, with stable angina, what does this mean to you? What kind of changes? At the very beginning, we looked at the pathogenesis of an atherosclerotic plaque. Remember that. 05:26 We talked about how there might be an endothelial injury. 05:29 We talked about how that was a thrombotic event. 05:31 We now also refer to your monocytes coming in and the smooth muscle cells that are being recruited from the intima coming into the media and all of this is then forming a fibrious cap, and what happened in the middle? A necrotic core of LDL, foam cells and such. 05:46 If that atherosclerotic plaque continues to build and build and build, what may then happen? 90% occlusion. 05:55 We're moving towards, what kind of angina? Oh, boy. Unstable angina, what's that mean to you? "Hey doc, I'm having chest pain when even at rest." Not good. Now, this comes under what? This comes under the category of acute coronary syndrome. Is that clear? Is this a myocardial infarction? Not at all. Is that clear? Are you going to find elevated cardiac enzymes? What's your gold standard please for cardiac enzyme? You all should know troponin I, not C. Is that clear? Troponin I. 06:30 Are you going to find troponin I with unstable angina? Yes or no? Good. No. Is that clear? Is it that crystal clear for you to differentiate between unstable angina, aka crescendo. 06:46 What are you crescendoing towards? You're crescendoing towards leaving this planet. 06:51 What does that mean? It means you're moving towards myocardial infarction. 06:54 You don't want that. Is that clear? So another name for unstable angina, you'll never forget that, will you? Laugh a little bit. You must chuckle. 07:02 You have a crescendo, you're moving towards a myocardial infarction. 07:06 How can you tell the difference? In myocardial infarction, obviously, the gold standard, cardiac enzyme is troponin I. 07:14 In unstable angina, yes, you're going to have chest pain at rest, but this is not a myocardial infarction, and you can confirm that how? Without finding any cardiac enzymes. Are you going to find changes on EKG? You could. It's called a non-STEMI, alright? So we'll talk about this. 07:33 Now, I want you to take a look at acute coronary syndrome. 07:35 Are we clear about definitions? Are we clear about concepts? Can we now understand what's going on from the beginning of the lecture series up to where we are right now? It's all about building up this information so that you integrate, across the board, from biochemistry or physiopath because that's what medicine is. 07:50 There's a type of questions and there's a type of patients that you're going to -- they're the type of patient that are walking through the door all the time. 07:58 Symptoms at rest. Number one: minimal exercise, perhaps, May not be relieved by nitrates because it's really beyond the point of that type of therapy. 08:08 Classified based on ECG changes, Now, it can be STEMI or non-STEMI. 08:13 If it's non-STEMI, we'll talk about that being perhaps an ST depression. 08:16 A STEMI is ST elevation myocardial infarction, and we will get into further detail. Not to worry at this point. 08:24 Next, the distinction, this is essential for management, is reperfusion therapy or not, is dependent on whether or none your patient has STEMI. 08:34 Now, reperfusion is another topic that we'll have to go into further detail when the time is right. 08:39 This is all under acute coronary syndrome. 08:41 I'm gonna keep repeating that so that you'll clearly know where we are. 08:44 What's your mainstay of treatment? Okay, now, so you have a clot. A clot is rather large, 90% perhaps. Let's do antiplatelet therapy. 08:53 Let's do anticoagulants. Let's do, maybe, the drugs aren't working properly and you have to get in their percutaneous. 09:01 You have to get in there with what's known as angioplasty. What does angioplasty mean? That type of intervention, percutaneous type of intervention. Angioplasty is ballooning, isn't it? Maybe place a stent. Maybe, just maybe, in that cath lab, your cardiologist is not able to get in there, put in a stent, which your only step in management at this point. 09:25 Next step in management, CABG, coronary artery bypass surgery. Let's continue. 09:31 Now, if it is STEMI, ST-elevation myocardial infarction, what do you do? Fibrinolysis. What does that mean to you? You have your reperfusion type of issues that we'll talk about. 09:42 That is something we have to discuss in greater detail. 09:46 Next, acute coronary syndrome, myocardial infarction. 09:50 What are the complications that you're worried about post-MI? Well, number one complication, worry about arrhythmias, aren't you? Therefore, you want to try to give your patient antiarrhythmics. 10:01 Now post-MI, let it be your boards. 10:03 Now clinically, it might be a little bit different, but remember antiarrhythmics are quite a complicated topic, isn't it? Now, we will deal with the little bit and right now, your first introduction post-MI arrhythmia, your best drug to give is something like your class 1B drug. B for best. 10:24 In general, when you say class 1 antiarrhythmic, then, what channel are you blocking, please? Sodium channel. Good. What kind of sodium channel? Voltage-gated or ligand-gated? How important is that? Really important from physio. It's your voltage-gated sodium channel. 10:41 Is that clear? This is something that you will be talking about and have discussed in pharmacology. 10:45 All I'm doing is reiterating it and clearly see where to bring all this information into play. 10:51 Next, beta blockers perhaps post-MI. Think about metoprolol. 10:56 Antiplatelet therapy drugs such as statin and so forth. 11:00 Also, what else are we worried about with myocardial infarction and as being a complication? How about congestive heart failure? If it is congestive heart failure, then you do everything in your power to decrease the mortality, increase survival, and there's a type of drug that you're looking for, aren't you? Therefore, those include spironolactone, metoprolol. 11:21 You're also looking at drugs such as ACE inhibitors. 11:25 Now, mainstay of treatment. Eventually, is the fact that you're trying to decrease the demand of oxygen by the heart. 11:31 You're trying to increase the supply of oxygen continuously. 11:34 Nitrates, perhaps and eventually, once you get past to hurdle and the emergency has been properly managed, then you get into lifestyle modification. Is your patient obese? Is your patient a smoker? Those things that you cannot control but you must educate your patient with include the fact that you have familial issues. 11:56 The beautiful, beautiful slide, the beautiful little explanation, a table in which it gives you a -- really, a storyline between stable angina moving into myocardial infarction, and we will get into further detail as we move through here.
About the Lecture
The lecture Acute Coronary Syndrome by Carlo Raj, MD is from the course Ischemic Heart Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
Which leads on the electrocardiogram most commonly show ST-segment elevation in the proximal occlusion of the left anterior descending artery?
- V2-V6
- aVL, aVR, aVF
- I, II, III
- II, III, aVF
- aVR, V1
How does sublingual nitroglycerin primarily reduce pain in angina?
- Venous vasodilation reduces preload
- Venous vasodilation increases preload
- Arterial vasodilation increases preload
- Arterial vasodilation decreases preload
- Arterial vasodilation increases afterload
Which of the following is most likely an acute coronary syndrome?
- Chest pain at rest
- Chest pain with lying down
- Chest pain with deep respiration
- Exertional chest pain relieved by rest after 2 minutes
- Sudden onset epigastric pain with maximum pain at onset plus epigastric tenderness
What type of channel is blocked by class I antiarrhythmics?
- Voltage-gated sodium channels
- Potassium channels
- Slow calcium channels
- Ligand-gated ion channels
- Beta-adrenergic receptors
What is the major difference between unstable angina and a myocardial infarction?
- Cardiac troponins are elevated in myocardial infarction.
- Cardiac troponins are elevated in unstable angina.
- ST-segment depression is never observed in unstable angina.
- ST-segment depression is observed in myocardial infarction.
- Chest pain begins with maximum intensity in myocardial infarction.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Best ACS diagram ever! Clear, concise, and delivered with enthusiasm.