Playlist
Show Playlist
Hide Playlist
Pneumonia: Diagnosis
-
Slides 01 URTIBronchitisPneumonia RespiratoryAdvanced.pdf
-
Download Lecture Overview
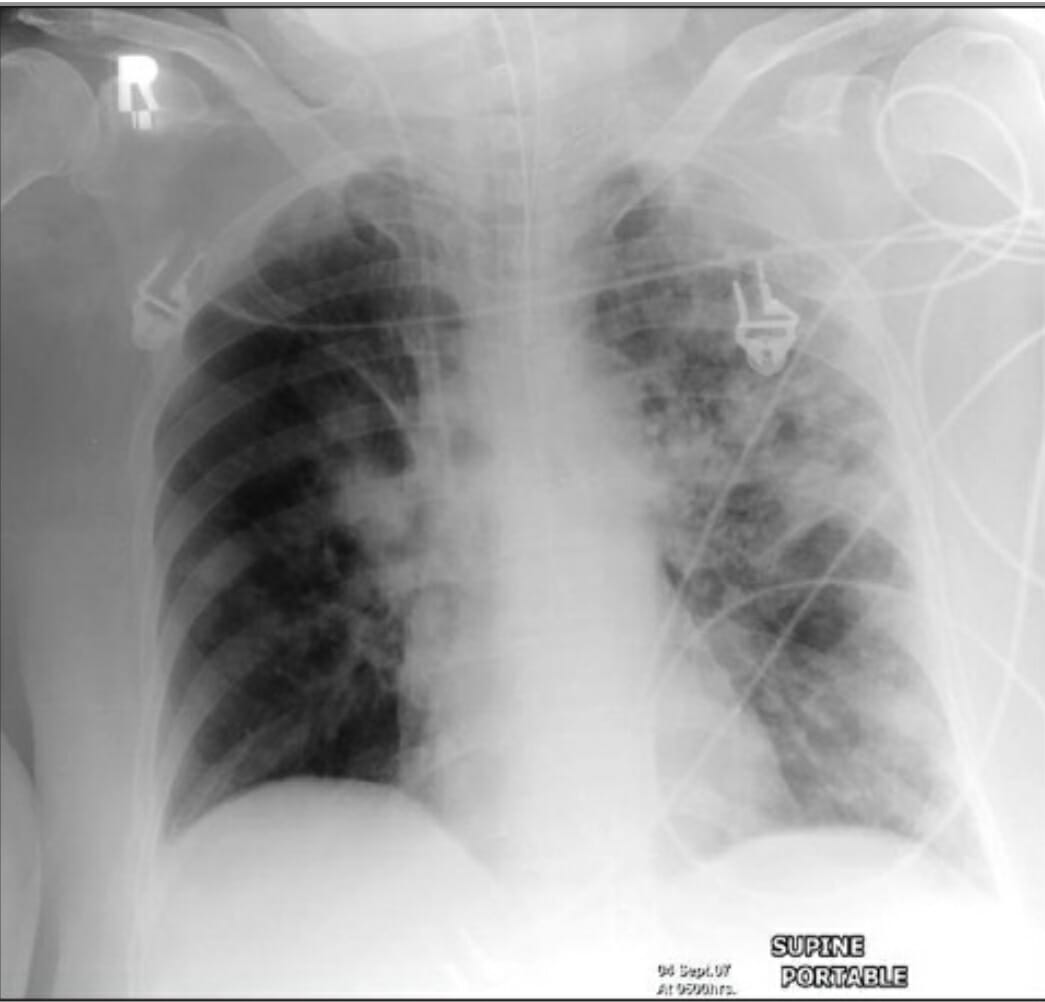
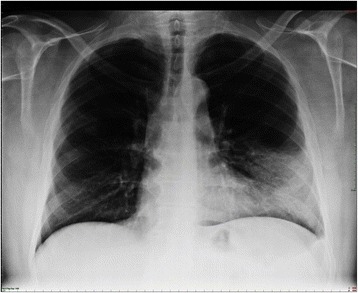
00:00 So, what are the principles in management as somebody who's presenting what seems to be a community-acquired pneumonia? Well, first of all, you need to confirm the diagnosis. 00:09 Then, you need to assess the severity, and then, you need to think about treatment and that has three main components to it. 00:16 Correct the oxygenation because that's the risk for mortality. Treat the fluid balance. 00:21 Again, hypertension is a risk for the patient, and three, clearly, it's an infection and you need to kill the pathogen and that's gonna require antibiotics. 00:31 And then, you need to monitor to make sure the patient's improving with whatever management you've instigated. 00:38 So, let's take these in turn. Confirming the diagnosis. Essentially, that's a chest x-ray. 00:43 You think the patient has some crackles over the right lung and they're presenting with a fever. 00:48 Then, you need to know whether there's consolidation present, so do a chest x-ray and it might show lobe consolidation as it's shown here on the right lower lobe in this chest x-ray. 00:56 It's also very important to do a chest x-ray to look for complications and we'll discuss some of those later in this talk but we're talking largely about pleural effusion and there may be related pathologies. 01:08 So, for example, if you have a lung tumor which is blocking a bronchus, then, you'll get pneumonia distal to that, distal to that obstruction quite easily. 01:19 So, a chest x-ray might help identify patients who have coexistent pathology which is relevant such as a lung cancer and, also, it will help confirm that there isn't another diagnosis present and that you've been fooled and this is not a pneumonia, for example, pulmonary edema or etc. 01:35 Sometimes, you might need to do more extensive radiological investigation such as a CT thorax or a CT pulmonary angiogram but that's unusual and if you're really worried about heart disease, then, you're gonna just do an ECG, echocardiogram. 01:49 Now, blood tests are quite useful in patients with pneumonia because there is certain abnormalities that may show up. 01:57 For example, if somebody's got an acute infection, you might expect the white cell count to go high, to be raised as an inflammatory response. 02:04 That's true. It happens a lot in pneumonia but also, a low white cell count is also characteristic of infection in these patients as well. 02:12 The urea and electrolytes can show a significant abnormalities are commonly a raised urea and a raised creatinine due to a degree of acute kidney injury. 02:23 And often, patients have a low sodium as well, a hyponatremia. 02:26 Liver function tests often are abnormal in patients with pneumonia, a high ALT and a high alkaline phosphatase and the albumin is one of those markers of acute infection. 02:36 So, for example, somebody gets acute pneumococcal pneumonia, their albumin may drop from its normal range of about 40 down to 25 very quickly. 02:45 So, hypoalbuminemia is a mark of infection. 02:49 Additionally, hypoalbuminemia is associated with increased severity, longer hospital stay, admission to the ICU, mechanical ventilation and increased 30-day mortality. 02:59 Possibly, the most important blood test is the C-reactive protein. This is a marker of inflammation. 03:04 So, if you have pneumonia, it's infection that should be a very significant inflammatory response. 03:09 So, the C-reactive protein which is normally less than five goes up very rapidly in most patients with pneumonia. 03:16 In fact, it's not uncommon for it to be above 100, 200, and even 500 or 600 patients of acute pneumonia. 03:23 The other blood tests we need to do are tests for oxygenation which I'll discuss later and there are some blood tests which are tests for potential infecting pathogens which I'll also discuss later. 03:35 So, what's the differential diagnosis of somebody presenting with what you might think is community-acquired pneumonia? But we actually mentioned already acute bronchitis, influenza bronchitis are two of the main differential diagnosis. 03:47 The important thing there is they do not normally have evidence of consolidation. 03:51 If you have evidence of consolidation either clinically or on x-ray, then, that means the patient has a pneumonia rather than just a simple, acute tracheal bronchitis. 03:59 Then, there are a range of common non-infective respiratory diseases which really need emphasis on anybody presenting with an acute, respiratory problem. 04:08 Pulmonary emboli, pulmonary edema, acute respiratory distress syndrome, not that common but very important, and lung cancer. 04:16 Now, the top two, pulmonary emboli, pulmonary edema, their common causes are acute respiratory problems and they're non-infective so that you should be able to distinguish in most patients with pneumonia from those but if you look at the data, many patients with pulmonary emboli are misdiagnosed with pneumonia initially, and the same for pulmonary edema. 04:36 So, that needs to be considered in differential diagnosis. 04:39 Lung cancer, because of its ability to cause infection distal to where lung cancer may be obstructing the bronchus needs to be thought about, especially, in the patients who are over 50 who smoke. 04:50 Just think, there may be a lung cancer underlying this problem or that the x-ray is showing, that you're seeing is not consolidation but a large tumor instead. ARDS is the subject of another lecture. 05:01 It presents with bilateral consolidation and marked hypoxia, and is actually a consequence of pneumonia frequently. 05:10 It can also occur in the situations where there is -- without pneumonia and has a relatively common presentation of bilateral consolidation which might be confused with pneumonia in some certain circumstances. 05:24 In addition, there are a range of relatively unusual and rare lung conditions which cause inflammation and consolidation or what looks like consolidation or an x-ray. 05:34 And these, because they cause inflammation and systemic upset, and have x-ray changes suggestive of consolidation could easily be confused with pneumonia. 05:42 Now, fortunately, they're very rare but they do need to be considered in patients who are not improving. 05:47 So, these include diseases such as cryptogenic organizing pneumonia, a non-infective form of consolidation, pulmonary eosinophilia, that's where you get eosinophil forming consolidation in the lungs, allergic bronchopulmonary aspergillosis which is a subject of one of the airways talks, hypersensitivity pneumonitis, and vasculitis which are discussed in the institutional lung disease talks and pulmonary vascular talks respectively. So, for example, this is a patient, is 40-year old man. 06:18 He's had two weeks of fever and breathlessness and a C-reactive protein shows this quite active inflammation with a CRP of 222. 06:26 Now, not unreasonably, he's been treated with antibodies because it's thought that he may have an infection, a pneumonia, but he's not getting better. 06:34 And in fact, it turns out that he has a disease and you can see this here which is causing a eosinophilic infiltration, a consolidation in both lungs as outlined by these -- the circles there, and this disease is called pulmonary eosinophilia and the treatment that's required in these circumstances is corticosteroids, and with that, he gets better. 06:56 So, this is an unusual disease but is an example of what could be confused as community-acquired pneumonia. 07:03 But I just have to reiterate, these are rare diseases and are only really considered in patients who are not getting better with antibiotics. 07:11 Management, how do we assess the severity? And this is largely done using a score called the CURB-65 score and this takes the five factors of confusion whether it's present or not, a urea whether it's greater than seven or not, a respiratory rate whether it's greater than 30 or not, blood pressure with a diastolic blood pressure is less than 60 or not and whether the patient is over 65 years age or not, and that gives you a six point score, not one, two, three, four, or five. 07:43 And with that score, that defines how severe or defines the mortality, the chance of death occurring with that episode of pneumonia. 07:53 For example, if the score is zero, the 30-day risk of dying is less than 3%. 07:58 That's a mild disease and most of these patients can be treated as an outpatient. 08:03 With a score of one or two, which is moderately severe, most of these patients will need to be hospitalized on a general medical floor. 08:10 A score of 3 or more signifies very severe disease, with a high 30-day mortality risk, Then, as the score goes up, the mortality associated with the score becomes higher, The pneumonia severity index or PSI is a validated clinical prediction model that is both more complex and accurate. 08:27 It stratifies patients into 5 risk groups, using 20 variables from 5 categories including demographics, medical history, physical examinan, laboratory results, and imaging. 08:38 It should be noted that clinical justment still plays a critical role in caring for these patients, but the PSI can be helpful to guide management. 08:45 As well as the CURB-65 Score, there are other features that can be used, other clinical features that can be used to identify patients who may have more severe disease. 08:55 So, worrying features of those are hypoxic despite having a high inspired oxygen concentration, patients who seem to have bilateral disease or disease that spreads during the hospital admission despite the antibiotics. 09:09 If somebody has a blood culture which is positive for an infected organism, that instantly places it into a group that has a mortality of about 20%. 09:17 The C-reactive protein, the blood marker for inflammation, if it's particularly high, above 250. 09:23 That seems to suggest patients who have an increased mortality in some data that's been published. 09:29 And then, if you have a severe comorbidity, if you have underlying cardiac disease, underlying COPD, or renal impairment, then, that is quite likely to decompensate because of the acute infection and that will increase the risk of severe consequences of the infection. 09:45 So, just to go for a couple of examples. 09:49 Here's patient A, age 53, presents to casualty with feeling with cough and phlegm, and fever for the past three days. He's not confused. 09:59 Urea was actually slightly high, a 9.8, but not terribly breathless. Blood pressure was normal. 10:04 That gives a CURB-65 score of 1 just for the urea alone. The rest was normal. 10:10 So, that's a 3% mortality. They're not hypoxic. 10:14 Chest x-ray confirmed pneumonia, but, actually, they could be treated at home with some oral antibiotics. 10:21 Patient B on the other hand is 67 years of age. 10:25 So, he gets a point for that and he's confused, so, he gets a point for that because normally, patients are not confused. He has a urea of 10, so, he gets a point for that. 10:35 He is breathless and his respiratory rate is 30, so, he gets a point for that. 10:39 He does not have hypertension, so, he does not get a point for that. 10:43 His total points give him a CURB-65 Score of four, and that suggests a mortality of about 28% for this type of patient. 10:51 In addition, his respiratory rate was above 30. 10:54 The PaO2 was low, it was less than eight, despite the patient being on 60% oxygen and there was bilateral consolidation. 11:01 So, this is a severe disease that is markedly hypoxic. 11:05 The patient needs to go to intensive care and probably needs to be intubated. 11:09 At least, if there's not an easy, quick response to high flow oxygen, the patient will need to be intubated and ventilated because of marked hypoxia. 11:18 In this situation, the patient actually survived. 11:21 Although, given the severity of illness, it was touch and go.
About the Lecture
The lecture Pneumonia: Diagnosis by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Infections of the Respiratory Tract.
Included Quiz Questions
Which of the following is NOT a reason to obtain a chest X-ray in a patient with dyspnea, asymmetrical crepitation, and dullness on chest percussion?
- To calculate the patient's CURB-65 score
- To identify consolidations
- To identify pleural effusions
- To exclude pulmonary masses
- To exclude uncomplicated pulmonary edema
Which of the following is NOT a common laboratory finding in a patient with pneumonia?
- Decreased C-reactive protein
- Decreased sodium
- Elevated WBC count
- Elevated urea and creatinine
- Decreased albumin
A patient presents with fever, chest pain, and difficulty breathing. Labs show markedly elevated WBC count, low serum albumin, elevated urea and creatinine, and elevated liver function tests. Chest X-ray appears clear. Which finding in the patient's initial evaluation does not fit with the diagnosis of pneumonia?
- Clear lung fields on chest X-ray
- High WBC count
- High ALT
- Low albumin
- High urea and creatinine
Which of the following is NOT a worrisome feature in the assessment of the severity of pneumonia?
- C-reactive protein < 40 mg/L
- Worsening consolidation
- Septicemia
- Presence of severe comorbidity
- Oxygen saturation < 92%
A 45-year-old male patient has been diagnosed with pneumonia. The patient is well oriented to time, place, and person. The patient's respiratory rate is 18 breaths per minute, blood pressure is 120/80 mm Hg, oxygen saturation is 95%, and urea level is 8 mmol/L. What is the next best step in management?
- Discharge with appropriate antibiotic therapy.
- Discharge with instructions for supportive care only (rest, hydration, etc)
- Admit and treat with broad-spectrum antibiotics.
- Admit to the intensive care unit for intubation.
- Observe the patient in the emergency department for 6 hours for deterioration in condition.
Which of the following does NOT indicate higher severity based on the CURB-65 scoring system for pneumonia?
- Respiratory rate < 30 breaths per minute
- Confusion
- Urea > 7 mmol/L (19 mg/dL)
- Diastolic BP < 60 mm Hg
- Age > 65 years
A 65-year-old man comes to the office with a 1-month history of chest pain and shortness of breath. The patient has bilateral crackles on examination and chest X-ray shows bilateral peripheral lung infiltrates with normal findings in central areas of the lungs. C-reactive protein is 230 mg/dL. The patient has been taking antibiotics for a month, but not responding to treatment. Which of the following is the most likely diagnosis?
- Pulmonary eosinophilia
- Lobar pneumonia
- Acute bronchitis
- Influenza
- Upper respiratory tract infection
A patient previously diagnosed with pneumonia presents post treatment with persistent signs and symptoms of septicemia. Based on the information from this lecture, what is the mortality percentage for patients with a similar presentation?
- 20%
- 10%
- 5%
- 50%
- 1%
Which of the following is TRUE about the CURB-65 score?
- The maximum CURB-65 score is 5.
- The risk of patient mortality increases as the CURB-65 score decreases.
- The CURB-65 score is the only method of assessing mortality in a patient with pneumonia.
- The CURB-65 score uses oxygen saturation as an important parameter in severity distinction.
- The CURB-65 score uses the same variables as the Pneumonia Severity Index (PSI).
What is the CURB-65 score for a 72-year-old man presenting with pneumonia, confusion, diastolic BP of 72 mm Hg, respiratory rate of 28 breaths per minute, and urea of 12.5 mmol/L?
- 3
- 2
- 4
- 5
- 6
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Well-explained, well-organized, and easily comprehensible. It covers all the important information in detail, labs, DD, assessment of severity.