Playlist
Show Playlist
Hide Playlist
GI Case: 33-year-old Man with a 10-week History of Diarrhea
-
Slides Gastroenterology 02 Diarrhea.pdf
-
Download Lecture Overview
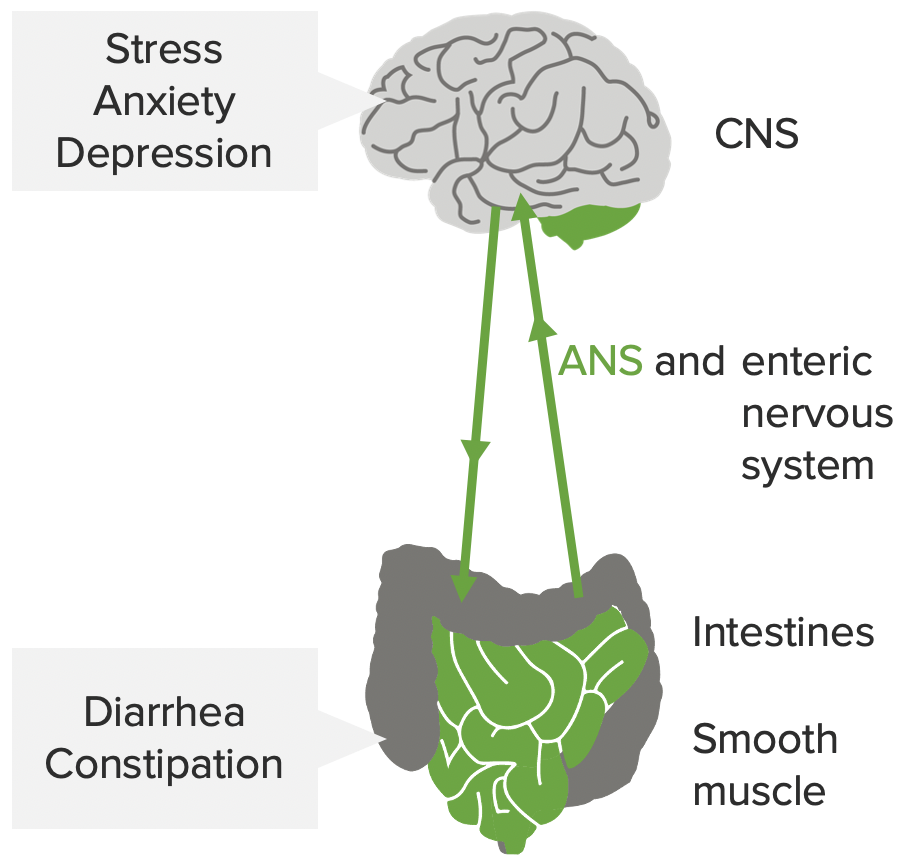
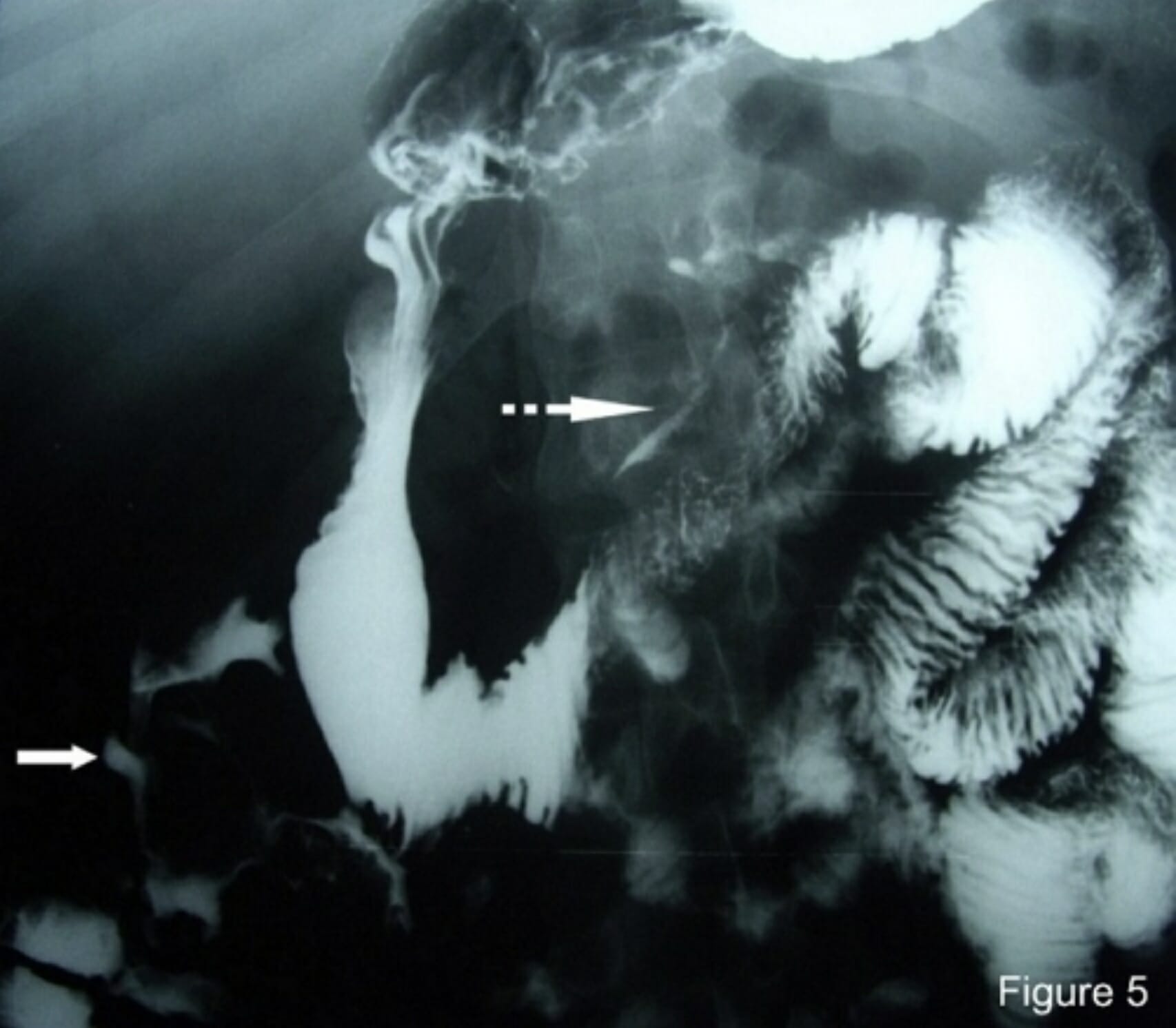
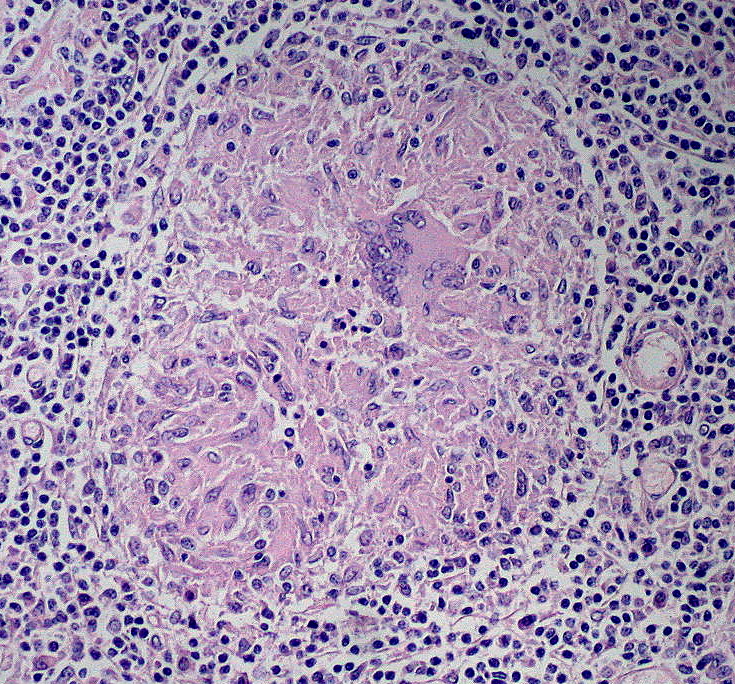
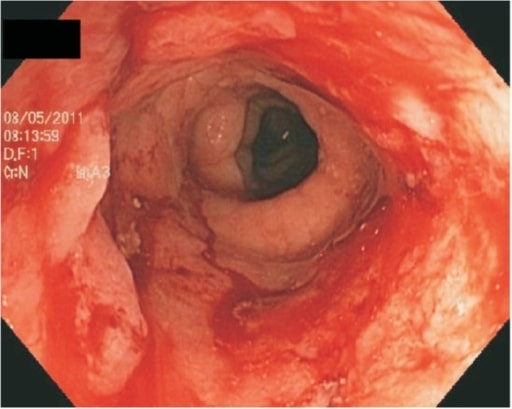
00:00 Let's move to our next case. 00:03 A 33 year old man is seen in clinic for a 10-week history of diarrhea and worsening abdominal crampy pain. 00:10 He has 6 to 8 bowel movements a day, including a few at night. 00:14 His stools are loose with streaks of blood and he has poor appetite and nausea but no fever. 00:20 He does not take any medications. 00:23 On exam, he is afebrile with a heart rate of 100 and blood pressure of 95/50. 00:30 His abdomen is soft with moderate diffuse tenderness in the lower quadrants with no rebound or guarding. 00:37 Colonoscopy shows patchy colitis with deep ulcers in a cobblestoning appearance and there is no involvement of the rectum. 00:46 So, what is the most likely diagnosis here? Let's look at some clues in this case. 00:52 So he has chronic diarrhea. 00:56 The presence of blood in the stools indicates that he may have an inflammatory diarrhea. 01:01 On his physical exam, he is tachycardic and mildly hypotensive which indicates probably, signs of mild hypovolemia. 01:09 And there is some keywords on his colonoscopy report such as cobblestoning and rectal sparing. 01:17 So, we put this altogether, he has chronic, bloody diarrhea which should automatically raise your suspicion for an Inflammatory Bowel Disease. 01:26 In addition, his colonoscopy report with patchy colitis and cobblestoning with rectal sparing should prompt you to think about Crohn's disease. 01:36 So, let's talk a bit more about IBD. 01:40 There are 2 types of IBD, they are Crohn's disease and ulcerative colitis. 01:45 They have very common clinical features and that they can both present with hematochezia, abdominal pain and fever, weight loss, a sense of fecal urgency or tenesmus. 01:57 They can both also present with symptoms outside of the GI tract. 02:02 So things like jaundice, uveitis, arthritis and lesions on the skin. 02:09 For the diagnosis, you first want to rule out any infection that could be contributing to their symptoms. 02:15 So, you would check a stool culture, a C. difficile toxin and a stool ova and parasites. 02:22 You may next also look for signs of inflammation in the stool. 02:26 So, a C-reactive protein or CRP and an elevated sedimentation rate or ESR can be helpful to look for systemic inflammation. 02:35 A fecal calprotectin can also be helpful because this is an inflammatory marker inside the stool that can help you track progression of the disease. 02:45 Lastly, you may do a colonoscopy to look for the specific features of each disease. 02:51 The treatment depends on the type. 02:54 So let's go into specifically Crohn's disease. 02:58 Crohn's disease is a transmural inflammation that can affect really any part of the GI tract. 03:04 So, the symptoms or clinical features you may encounter are diarrhea, abdominal pain, basically any symptoms involving the intestine. 03:13 You may have rectal bleeding, in the stomach, they may have vomiting, and it can also affect the liver and bile duct leading to inflammation. 03:22 Outside of the GI tract, patients may have inflammation or uveitis of the eyes. 03:29 They may develop skin ulcers and sores, One typical rash that we see often is erythema nodosum. 03:36 They may also have systemic signs of fever, weight loss and anorexia or decreased appetite. 03:42 They may also have ulcers in the mouth. 03:46 These patients tend to have frequent flares and remissions of their disease. 03:50 And because of the transmural inflammation, so that's inflammation extending through the wall of the bowel, there are common complications such as fistulae and bowel obstructions. 04:03 Treatment is done with corticosteroids for flares and for maintenance therapy, we give immunomodulators such as methotrexate or more advanced biologic agents that target the anti-TNF pathway such as infliximab. 04:21 Most patients, because of their relapsing and remitting disease will eventually require surgery. 04:28 Now let's talk about ulcerative colitis. 04:31 So, unlike Crohn's disease which is a patchy inflammation involving any part of the GI tract shown here, ulcerative colitis is a continuous inflammation that involves the colon and the rectum as shown here. 04:47 It usually does not involve the small bowel and it is associated with diagnoses like primary sclerosing cholangitis, cholangiocarcinoma and higher rates of colorectal cancer. 05:01 The treatment as with Crohn's is with first, corticosteroids for flares. 05:07 For maintenance therapy, we also give 5-aminosalicylic agents like mesalamine. 05:13 and we also have immunomodulators and biologics for severe disease. 05:17 So you might be thinking at this point that a Crohn's disease and ulcerative colitis have a lot in common. 05:23 So how do we tell them apart clinically? These are some clues that can help you make the diagnosis. 05:29 So Crohn's disease, again involves inflammation of the entire bowel wall, so transmural inflammation. 05:37 Also, patients tend to have skip lesions, so patchy involvement and a cobblestoning appearance. 05:45 They often have spared areas on colonoscopy. 05:48 On the other hand, ulcerative colitis involves inflammation limited to the mucosa and the submucosa only. 05:56 and inflammation tends to be continuous, so there are no skip lesions. 06:03 The location also differs. 06:04 With Crohn's disease, this can involve any part of the GI tract. 06:08 It typically, however, spares the rectum. 06:11 And the terminal ileum is the most common site. 06:14 With ulcerative colitis, only the rectum and the colon are involved. 06:20 The last thing to distinguish between the two are the common complications. 06:25 So if you remember that Crohn's disease involves transmural inflammation then you'll remember that fistulae and abscesses are more common with this disease. 06:35 With ulcerative colitis, associated complications are a higher risk of colorectal cancer and the association with the diagnosis of primary sclerosing cholangitis.
About the Lecture
The lecture GI Case: 33-year-old Man with a 10-week History of Diarrhea by Kelley Chuang, MD is from the course Approach to Patients with GI Symptoms.
Included Quiz Questions
Which of the following complications is more commonly associated with Crohn disease than ulcerative colitis?
- Fistulae
- Primary sclerosing cholangitis
- Colorectal cancer
- Toxic megacolon
- Hemorrhage
Which of the following is more common in ulcerative colitis than in Crohn disease?
- Involvement of the colon and rectum
- Transmural inflammation
- Cobblestoning
- Fistulae
- Abscess
Which of the following is the treatment of choice for acute flares of Crohn disease?
- Corticosteroids
- Methotrexate
- Azathioprine
- Infliximab
- 6-Mercaptopurine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |