Playlist
Show Playlist
Hide Playlist
GI Case: 21-year-old Man with 6 Months of Diarrhea
-
Slides Gastroenterology 02 Diarrhea.pdf
-
Download Lecture Overview
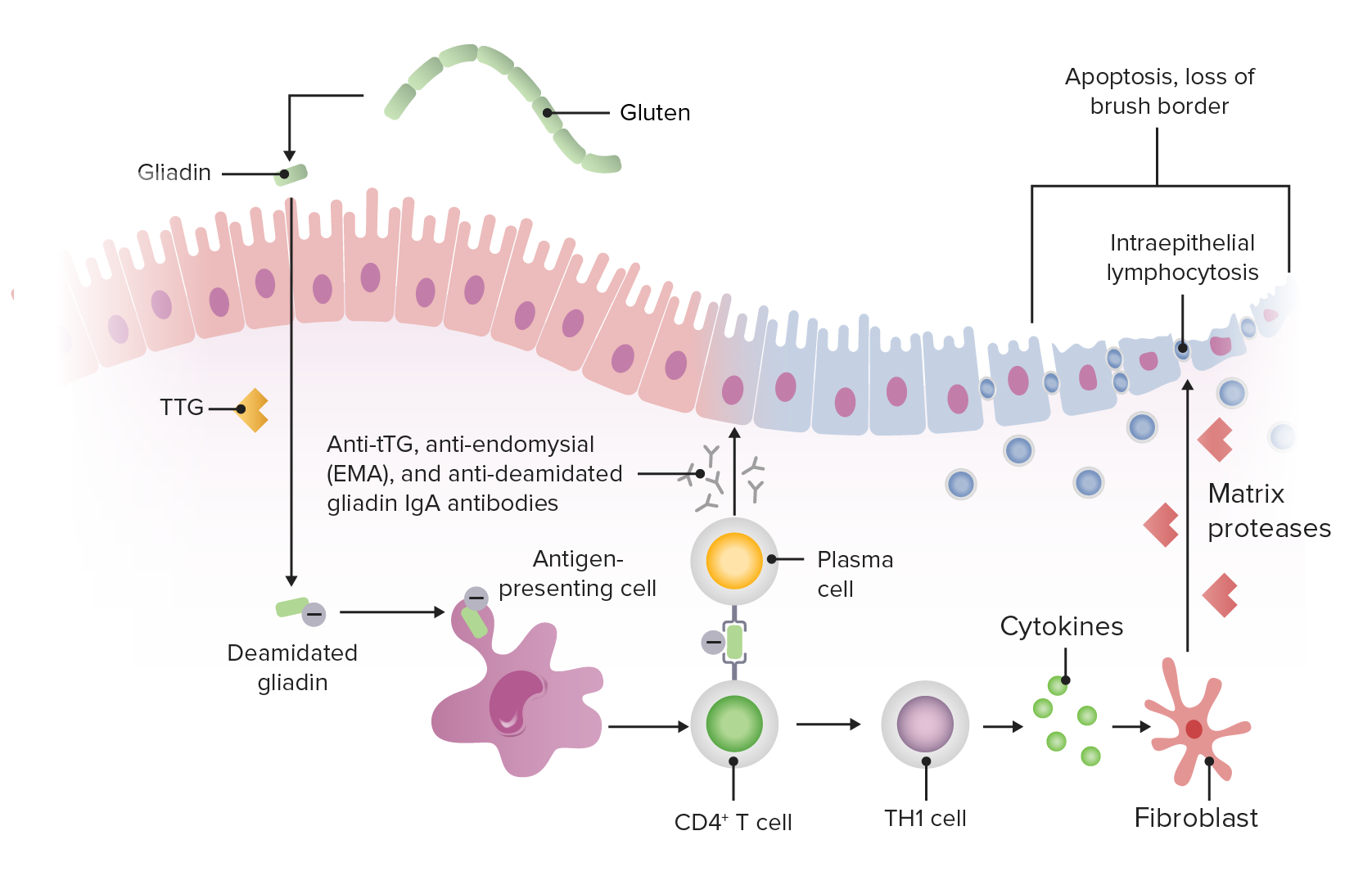
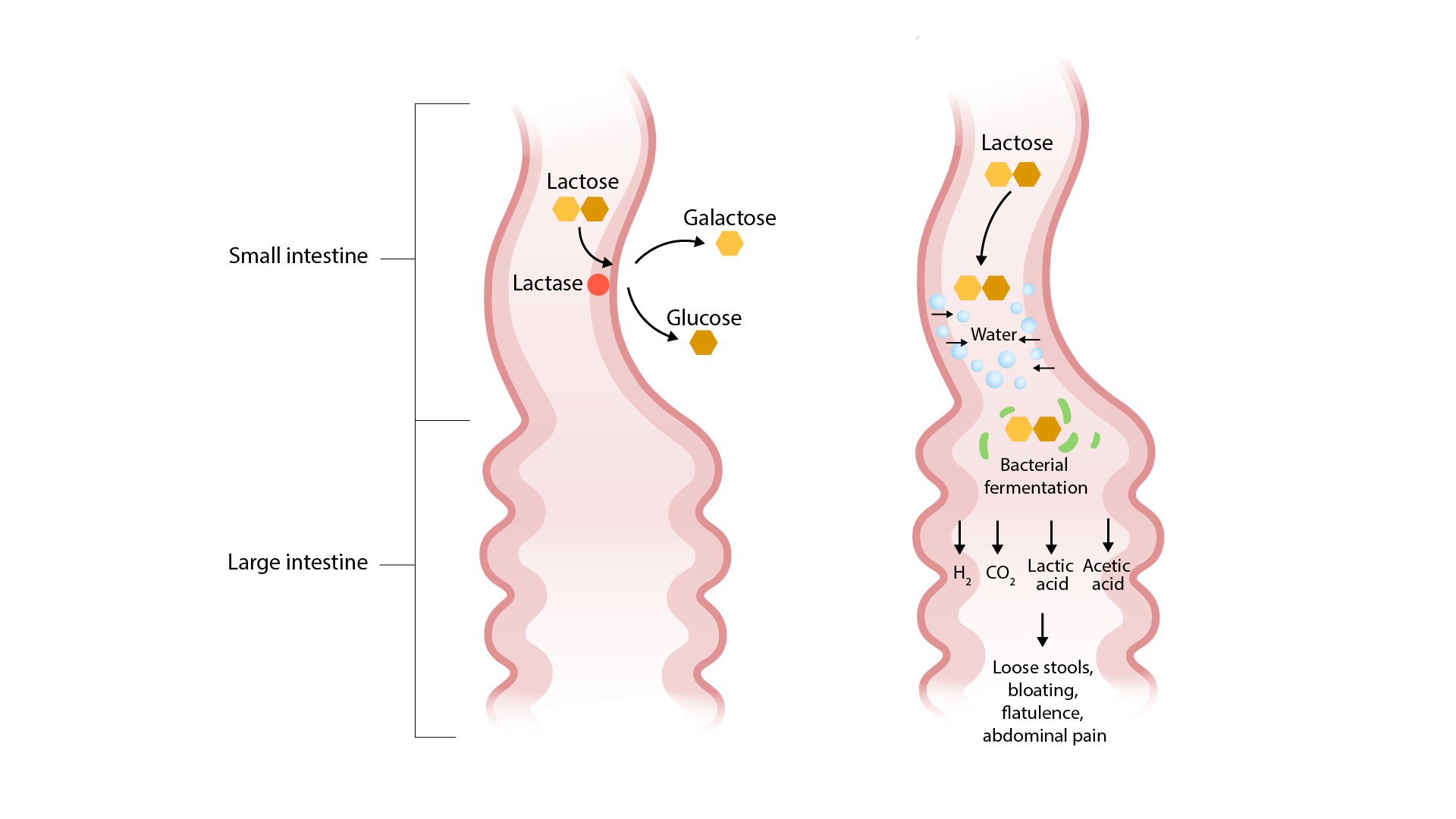
00:00 Now let's move to our next case. 00:03 A 21 year-old man with a history of type 1 diabetes presents to the clinic with 6 months of diarrhea. 00:09 He has had malodorous, loose stools about 4 to 5 times a day for the past 6 months. 00:15 Since the diarrhea began, he has lost 3 kgs unintentionally. 00:20 He has no fevers, recent travel, abdominal pain or blood or mucus in his stools. 00:26 On exam, vitals are normal, he appears thin. 00:30 His abdomen is soft and non-tender. 00:32 Labs show a hemoglobin of 11 with a mean corpuscular volume or MCV of 105. 00:40 So the question is, what diagnostic test should be done next? Before we answer that, let's look at some key clues here. 00:49 So, he has a history of type 1 diabetes which is a history of autoimmune disease. 00:55 He does have chronic diarrhea with unintentional weight loss. 01:01 And in this case, he has an anemia that is macrocytic so this might suggest a nutritional deficiency in an appropriate clinical scenario. 01:12 So let's now talk about chronic diarrhea. 01:16 We can break down chronic diarrhea into several different types. 01:20 The first type is called secretory diarrhea. 01:23 This distinguishing factor about secretory diarrhea is that it occurs at all times of day and night. 01:30 So that's an important question you should always ask your patients about. 01:35 The differential diagnosis for this includes things like Carcinoid syndrome, VIPomas and Zollinger-Ellison syndrome. 01:43 The next type of diarrhea is osmotic diarrhea or for malabsorption. 01:48 This tends to be associated with eating and because of that does not occur at night and can be associated with an increased stool osmotic gap which we will discuss later. 01:59 The differential diagnosis here is quite broad but includes things like lactose intolerance, pancreatic insufficiency and Celiac disease. 02:09 The next type of diarrhea is inflammatory. 02:12 Patients with inflammatory diarrhea tend to have bloody and mucousy stools and they may often have fever or systemic symptoms. 02:21 The differential diagnosis here are your types of inflammatory bowel disease like Crohn's disease and ulcerative colitis. 02:29 Lastly, we have a motility disorder. 02:32 Patients with motility-related diarrhea often have no alarm features and a normal colonoscopy. 02:39 An example of this type of disorder is Irritable Bowel Syndrome. 02:45 So now that we've categorized different types of diarrhea, let's now talk about a diagnostic algorithm for helping you differentiate between your broad differential. 02:56 So we begin with the patient presenting with chronic diarrhea, you want to first exclude any of the things listed here. 03:03 So anything that can cause acute diarrhea - lactose intolerance, irritable bowel syndrome, a prior history of gastric or ileal resection, a parasite infection, medications that can cause diarrhea and any systemic diseases. 03:19 Keep in mind that much of this work up you may be doing simultaneously. 03:25 Once you have done those things, you could then send appropriate initial testing. 03:29 So this may include things like a fecal calprotectin which is an inflammatory marker in the stool. 03:36 You can also check for occult blood and you may also do a colonoscopy or imaging of the small bowel to further investigate. 03:44 If any of those things are abnormal, you should then work up that patient for inflammatory bowel disease or cancer. 03:51 If they are normal on the other hand, then we must do further testing. 03:56 So, that further testing involves checking a stool osmotic gap. 04:02 We will discuss exactly what goes into this measurement a bit later. 04:06 If you have an increased osmotic gap, the next thing you wanna check is the fecal fat content. 04:13 If you have high fecal fat, this indicates that the patient has a malabsorption syndrome such as pancreatic insufficiency or bacterial overgrowth. 04:24 If they have normal fecal fat, then your differential includes things like lactose intolerance, sorbitol or lactulose or laxative abuse. 04:35 Now, if your patient had a normal osmotic gap, the next thing you can use to differentiate between causes is a stool weight. 04:44 So, if they have a normal stool weight, this makes your differential limited to things like Irritable Bowel Syndrome or factitious diarrhea. 04:53 If the stool weight is quite high or greater than a 1000 grams in 24 hours, this suggests that your patient may have secretory laxative abuse. 05:06 So, we mentioned earlier a malabsorption syndrome. 05:09 A malabsorption syndrome is the inability to absorb nutrients due to some underlying condition. 05:15 The most commonly involves the small bowel because that's the location where we absorb the majority of the nutrients we take in. 05:23 So what are the mechanisms by which malabsorption can occur? There are several different mechanisms that we'll review here. 05:30 The first is impaired mucosal absorption as in Celiac disease or Whipple disease. 05:37 Next, you may have an issue with your brush border enzymes, so such as in lactose intolerance. 05:46 If you have a problem with your pancreatic enzymes or pancreatic insufficiency, you may have chronic pancreatitis or pancreatic cancer. 05:56 Next you may also have issues with bile acid circulation. 05:59 An example of an underlying cause here is an ileal resection. 06:04 And lastly, bacteria play a very large role in helping us digest our nutrients. 06:09 So, when you have overgrowth of certain bacterial species, you may also develop malabsorption. 06:14 An example here is small intestine bacterial overgrowth. 06:19 So earlier, we also mentioned a stool osmotic gap. 06:23 This is a simple measurement you can do by first measuring the stool sodium and the stool potassium. 06:30 And then with this calculation, this will help you differentiate between secretory and osmotic diarrhea. 06:37 When the stool osmotic gap is less than 50, this suggests a secretory diarrhea. 06:43 Between 50 and 125, this is an indeterminate finding, so that is not quite helpful. 06:49 But if it is greater than 125, this helps us because it suggests an osmotic diarrhea. 06:56 Let's talk a bit more specifically about one of these types of malabsorption, Celiac disease. 07:02 Celiac disease is an immune mediated reaction to gluten and gliadins in our food. 07:07 Patients tend to present with weight loss, they may have fatty stools or steatorrhea and because of their inability to absorb fatty nutrients, they may also have nutritional deficiencies. 07:22 The diagnosis is done by testing for specific antibodies. 07:26 So those are the anti-tissue transglutaminase (TTG) or the anti-endomysial (EMA) antibodies. 07:35 The diagnosis can also be made by endoscopy or colonoscopy. 07:39 Here, the features all point out here in our example of histology from a patient with Celiac disease is villous blunting, so blunting of the villi, and infiltration of lymphocytes into the epithelium, as shown here. 07:55 The treatment is simply done by avoiding gluten in the diet. 08:02 So now that we've previewed all of that, let's return to our case. 08:07 A 21-year old man with a history of known autoimmune disease is now coming with chronic diarrhea, unintentional weight loss. 08:15 and some of the clues in his labs show that he has a macrocytic anemia which might suggest a nutritional deficiency. 08:24 In addition, one further clue is that he has malodorous stools which may be a sign of steatorrhea or malabsorption. 08:34 So what diagnostic test should we do next? Because he is young and he has the presence of another autoimmune condition, you should suspect Celiac disease in this case. 08:45 And the diagnosis can be made with sending an anti-tTG antibody serology.
About the Lecture
The lecture GI Case: 21-year-old Man with 6 Months of Diarrhea by Kelley Chuang, MD is from the course Approach to Patients with GI Symptoms.
Included Quiz Questions
Which of the following is the diagnostic test of choice for celiac disease?
- Test for anti-tissue transglutaminase antibodies
- Test for antimitochondrial antibodies
- Test for antinuclear antibodies
- Test for anticentromere antibodies
- Test for anti-Smith antibodies
Which of the following changes is expected in patients with secretory diarrhea?
- SOG <50
- SOG >50 and <125
- SOG >125
- SOG >200
- SOG >100
Which of the following describes the mechanism of malabsorption in lactose intolerance?
- Brush border enzyme deficiency
- Impaired mucosal absorption
- Decreased bile acid circulation
- Pancreatic insufficiency
- Bacterial overgrowth
Which of the following medical conditions results in an increased stool osmotic gap and normal fecal fat?
- Lactose intolerance
- Pancreatic insufficiency
- Irritable bowel syndrome
- Factitious diarrhea
- Malabsorption syndrome
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |