Playlist
Show Playlist
Hide Playlist
Respiratory Failures: Treatment
-
Slides RespiratoryFailure RespiratoryPathology.pdf
-
Download Lecture Overview
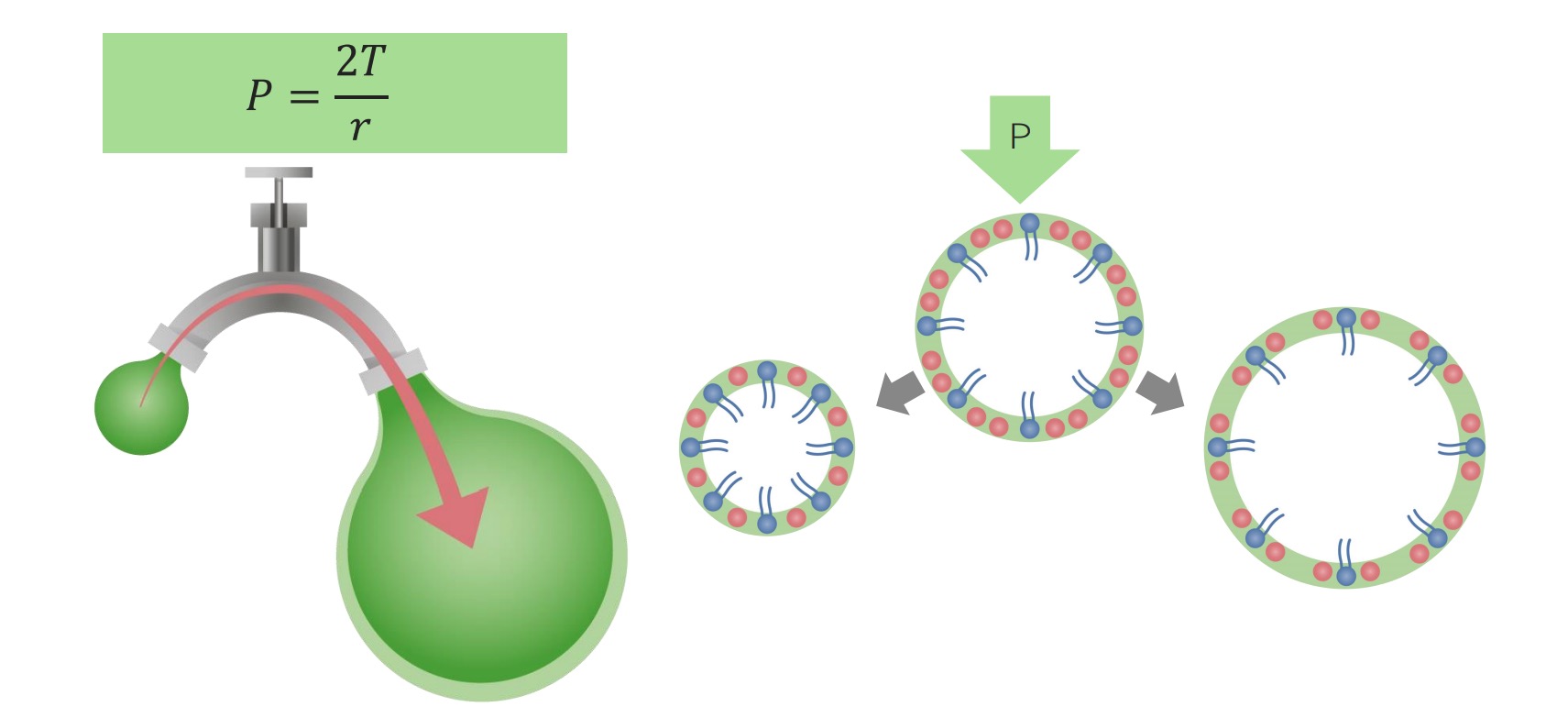
00:00 Now, treatment, all depends. I mean, this could be all over the place. 00:04 If your patient is suffering from issue such as asthma or COPD, then maybe you’re thinking about steroids. 00:11 But, if it’s pneumonia that’s resulting in chronic type of issues, maybe it’s antibiotics and with acute respiratory distress syndrome, here once again, well, ventilatory support, which is a highly hot topic for you on the boards. 00:27 Becomes important for at least, introduce a few ventilatory support assisted control type of modes of respiration. 00:37 You’ll see. 00:38 Continue. 00:39 Options include the following. 00:41 Oxygen, it’s not really ventilatory support, so you want to be careful here. 00:47 With oxygen, remember, if your patient is already accustomed to low oxygen and is breathing normally, and then all of a sudden, you introduce more oxygen, that could be a problem. 00:57 Be very careful. 00:58 Non-invasive. We’ll talk about in great detail. 01:01 These include your BiPAP or non-invasive type of ventilator. 01:04 NIV, it’s non-invasive ventilation here. 01:07 And intubation, of course, will be your mode, we’ve talked about that child who had respiratory muscles that then became tired and fatigued and therefore, resulted in retention of carbon dioxide and perhaps the death of the child. 01:22 So, we’ll talk about endotracheal ventilation, but mechanical ventilation becomes important. 01:27 Okay. Now, what are the indications for ventilatory support? What are they? Hypoxia. 01:33 PO2 of what? A 60. 01:35 Oxygen. 01:37 Next, hyperbaric or hypercarbic ventilatory support, when PCO2 is greater than 50 with the decreased pH. 01:44 You wanna be careful with that carbon dioxide being elevated. 01:46 Not a good thing. 01:48 So this is indications for various types of ventilatory support that we shall walk through. 01:53 Shock, major trauma, airway protection and much more important than any cut-off is your clinical impression of the patient. 02:01 But, that’s more about practice. 02:03 Let’s make sure that you are completely clear about what kind of gas values are the cut-off point for you to seriously start thinking about next step of management. 02:13 Ventilatory support. 02:18 Now, what about these non-invasive ventilations that you wanna be familiar with? We’ll walk through here a few and then, we'll take a little break from some of our modes and then when we get into our next topic, what we’ll do is we’re gonna hit that hard. 02:35 We’ll hit the modes especially, we’ll talk about the terminology and what it means. 02:39 But, here, let’s first begin by laying down the foundation. 02:42 So, CPAP is something that you wanna be extremely familiar with. 02:45 It’s continuous positive airway pressure. 02:52 A positive on purpose, because here, physiologically it’s important for you to understand. 02:56 Why? For the following reasons. 02:59 Normal breathing mechanics. 03:01 Tell me quickly, what happens to diaphragm upon contraction when you wanna inhale? Contract, moves downwards. 03:08 Good. 03:09 What’s your next step? The pleural pressure, which is how much? To begin with, you are at FRC. 03:16 Oh, boy. 03:18 Pleural pressure was negative, approximately -5. 03:21 With the diaphragm contracting and then now, the pleural pressure becomes more negative. 03:25 The more that your pleural pressure becomes negative, what happens to your lung? It expands. 03:32 Is that clear? In the meantime, there are a couple of things that this then causes. 03:37 So, upon let’s say from -5 to -8, your pleural pressure becomes negative. 03:42 Do you remember that from physio? Bring that here. 03:45 Next, as it does so, then what happens to alveoli? Its pressure becomes negative. 03:50 You’re gonna suck in the air, like a straw. 03:54 Clear? Clear. 03:55 In the meantime, what about that recoil force? The recoil force has to then equal that increased negative pleural pressure. 04:03 That’s just simple lung mechanics. 04:06 Think of it as being a straw sucking in all the different things that has to occur in order for that to happen. 04:13 That’s a negative pressure that’s doing what to alveoli? Expanding. And that’s my point. 04:19 In physio, you know that you have to cause a negative pressure, right? In order for your alveoli to expand. 04:27 Let’s say that the lungs cannot. 04:29 Say there is some kind of indication, maybe it’s the PCO2 being above 50, the PO2 being less than 60 mmHg. 04:36 Maybe there’s an indication or maybe your patient has obstructive sleep apnoea. 04:42 And at this point, you have to get ventilatory support. 04:46 This is going to come in the way of continuous positive airway pressure. 04:51 Keep that in mind. 04:52 You understand the significance now and how different this is than physio. 04:57 You will see the consequences coming up. 04:58 Used acutely more for hypoxic failure, CHF especially. 05:03 Commonly used chronically to stent open upper airway obstruction, especially sleep apnea. 05:10 Think of obstructive sleep apnoea, but the only way that you can keep it open is literally introducing positive pressure. 05:17 We’ll talk a little bit more. 05:19 BiPAP is bi-level positive airway pressure. 05:22 Used acutely for hypoxic and hypercarbic failure, very effective in COPD. 05:28 This would be the next step of management in terms of really being able to control the breathing of your patient. 05:34 Good evidence of support its use and how common is immunosuppressed patient? Quite common. 05:42 So, immunocompromised, immunosuppressed patients, let it be something like HIV, or, of course, on immunosuppressive therapy. 05:49 And you see more and more and more of these patients, so this becomes incredibly important for you. 05:53 This is known as BiPAP. 05:55 Bi-level positive airway pressure.
About the Lecture
The lecture Respiratory Failures: Treatment by Carlo Raj, MD is from the course Respiratory Failures.
Included Quiz Questions
Which of the following is an indication for ventilatory support?
- PO2 < 60 mm Hg on high-level supplemental oxygen
- PCO2 < 50 mm Hg with decreased pH
- PO2 < 80 mm Hg on high-level supplemental oxygen
- PCO2 < 50 mm Hg with increased pH
- Hypertension
Which of the following muscles flattens as it contracts during inspiration?
- Diaphragm
- External intercostals
- Internal intercostals
- Anterior scalene
- Sternocleidomastoid
Customer reviews
2,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text