Playlist
Show Playlist
Hide Playlist
Tophaceous Gout
-
Rheumatology I 01 Non-Autoimmune Arthritis.pdf
-
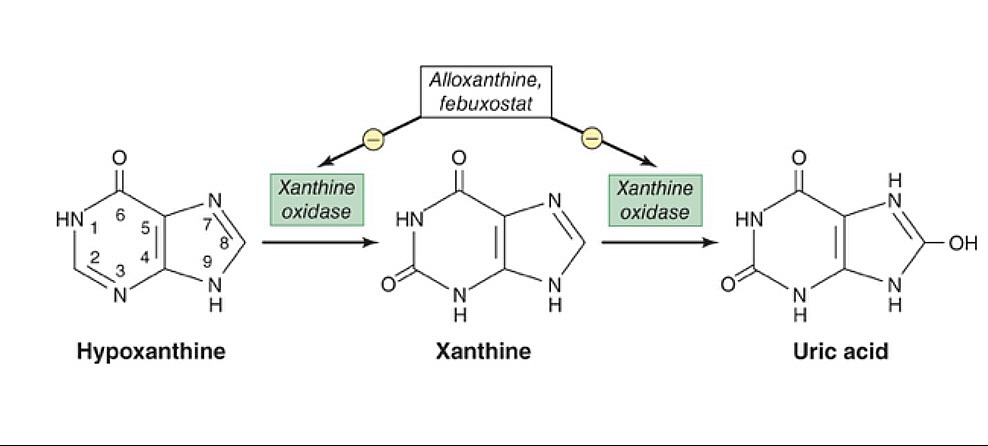
Download Lecture Overview
00:01 What if the uric acid accumulates in soft tissue? We call that tophi, or tophaceous gout. 00:08 Take a look at the pictures here. 00:09 Immediately show you the toe. 00:12 You see that toe? Inflamed like crazy, huh? You call that, what, podagra. 00:18 You'd find in there uric acid crystals. 00:21 Let's identify these uric acid crystals just to get ahead a little bit. 00:25 Once you possibly using polarized light, let me ask you a question. 00:29 That polarized light that you're trying to identify the uric acid, you think you'd find it to be negative or positive for birefringent? That we'll talk about in a little bit. Okay? Keep that in mind. 00:40 What if the uric acid accumulating in soft tissue? We no longer call that podagra, for example. 00:45 Think that maybe you might be accumulating in the elbow, or maybe as we see here, in the hands and such. 00:51 Do not confuse this with osteoarthritis. 00:54 Remind me, in osteoarthritis, what was it called when you had inflammation to the DIP? Oh, Heberden nodes, correct? Had nothing to do with uric acid. 01:02 What about in PIP? It's called Bouchard, and maybe the thumb. 01:07 However, osteoarthritis was non-inflammatory. 01:09 You did not have an inflammatory response, correct? So, as you move through rheumatology here, you're going to categorize the different arthritis, and what it comes under so that you can clearly understand how to deal with and identify each patient. 01:25 Recurrent episodes of the gout could eventually result into chronic. 01:28 By definition, though, is that what chronic means? Chronic usually means recurrent, recurrent, recurrent, acute, correct? There we have it. When you have recurrent issues, then may turn into chronic. 01:39 When it turns into chronic, oftentimes, maybe, it might be affecting your knees and such. 01:43 Keep that in mind. These flares. 01:47 Do you find a toe here? Well, let me tell you, the one on the left is your hand. 01:53 That's your fingers, all right? So therefore, you can't call that podagra. 01:58 Is that your toe? Uh, no. I think that's you're index finger. 02:01 Yeah, correct. So that is your tophi. 02:03 Or periauricular, around the ear. 02:06 It's the tophaceous gout or tophi. 02:08 Accumulation of what? Uric acid. 02:11 Remind me, on polarized light, what are we going to look for? So now, let me tell you, it's negative birefringent crystals. 02:18 But what does that mean? Well, I'll walk you through that in a bit. 02:23 Diagnosis. We're going to analyze arthrocentesis. 02:28 In the synovial fluid, we're going to find…here it is. 02:31 The uric acid crystals. It's needle- shaped. It's needle-shaped. 02:36 Not rhomboid. 02:39 Needle. If you don't know what rhomboid or… Rhomboid looks a little bit more like a square, a little bit larger. 02:44 If you want, look it up. 02:46 That's some geometry, but needle is what we're looking at here. 02:49 It's a negative birefringent. 02:51 So, if it's negative birefringent, what does that even mean? First know that you're going to be looking for polarized light. 02:59 With polarized light, it is the parallel nature of these needles that you're going to be looking for. 03:05 If you know that these negative crystals are negative for polarized light, is that mean that the color is blue or yellow, please? Yellow. Okay? Now, what does that mean? That means that you're going to be looking for yellow, needle-like crystals that are parallel. 03:25 That a parallel, I repeat. 03:27 So we have polarized light, we have parallel, and it's negative, which means that it will be yellow. 03:35 Which means if it's perpendicular type of light, then it'd be blue. 03:39 That is the definition of negatively birefringent. 03:43 Most important thing, the needles, polarized light, negative, yellow, parallel. Is that understood? We're going to compare this with what goes on with CPPD, which is calcium pyrophosphate deposition disease as we shall see next. 04:03 Diagnosis, hyperuricemia. 04:05 Well, you want to take a look at the underlying issue. 04:07 And, in fact, we know that uric acid levels could… seen during flares, most of the time. 04:14 So, usually, it can be immeasurable, so be careful with these flares during chronicity. 04:19 Only 10% of hyperuricemia patients truly develop gout. 04:22 That's another point that you want to keep in mind. 04:25 But, trust me, if the boards want you to know that this is gout, they're going to give you the classic symptoms in which you'd be able to identify. 04:33 However, you do need to make sure that you understand the difference between acute and chronic, especially, when we get into management. 04:42 So let's attack the acute gout in this patient. 04:46 What's that acute gout patient complaining of? Pain. 04:50 So much though, they can't even place a feather on their toe. 04:53 So therefore, NSAIDs, colchicine. Now, be careful colchicine, though. 04:59 Colchicine literally, is going to inhibit the migration of neutrophils towards that crystal. 05:05 In other words, it's like you're kind of creating Chédiak-Higashi, right? If you're with me, you're great. If not, no worries. 05:13 At this point, colchicine inhibits the migration of neutrophils towards your crystal. 05:18 So if you don't have the migration, you don't have phagocytosis, you don't have inlfammasome, oh, guess what? You don't have the pain. Nice job. 05:25 But with colchicine, the side effect profile is devastating, could be extremely severe. 05:31 Diarrhea, myopathy, and also as bad as pancytopenia. 05:35 Keep that in mind, please. The side effect profile is quite bad for colchicine. 05:40 Now, apart from that, oral steroids for patients who cannot tolerate NSAIDs or colchicine because now you're worried about a patient who comes in with kidney disease. 05:50 And on top of that, you're going to give colchine? Be careful. 05:53 Or even NSAIDs, for that matter, correct? Let's divide this into chronic. 05:59 In chronic, you may not even find high levels of uric acid. 06:04 So uric acid level might be low. 06:06 And then with chronic gouty attack, now at this point, you're not so much worried about the pain in the patient but it's the fact that you want to try to stop the synthesis of uric acid. 06:19 The drugs we have here is allopurinol or febuxostat. 06:24 In other words, you're going to stop the growth or stop, more or less, the enzymatic conversion, known as your xanthine oxidase. 06:35 So, if you inhibit that enzyme, now obviously, that takes a lot longer, right? So therefore you can't use allopurinol and febuxostat with acute gout. Is that clear? As we're dealing with chronic. 06:47 Now, especially if you're overproducers. 06:48 I gave you 1 example for overproducers and that was…? Good. That was the fact that I gave you tumor lysis syndrome. 06:54 Increase chemotherapy, increase destruction, increase release of uric acid, that's one. Number 2, what if you had a patient that was young and had hypoglycemia, had hepatomegaly. 07:06 Also had hypertriglyceridemia, and also had gout formation, and also had gout formation, did not have proper gluconeogenesis and glycogenolysis. 07:16 Put all that together for me and you're going to tell me about a particular condition that you know as being a type 1 glycogen storage disease, we call von Gierke. 07:26 There you might have overproduction. 07:28 So when you have over production, it's nice to have a tool, such as allopurinol, to inhibit that enzyme. 07:35 The goal is to bring your uric acid < 6 mg/dL. 07:41 If urinary uric acid > 1000 mg/day, patient at risk for acute obstructive uropathy, so be careful. 07:49 Should be started until several weeks after the acute gouty attack. 07:53 So, in other words, remember, you want to wait, and you want to take care of the pain first. 07:58 And then you want to try to inhibit the enzyme that will produce your uric acid. 08:03 Several weeks, please, is key there. 08:06 You'll need dose adjustment for chronic kidney disease. 08:08 Now, anytime that you have issues there, you're worried about allopurinol. 08:16 What about your allopurinol and, at this point, you still have high levels of uric acid? Now, these become quite interesting. 08:24 So now what you're going to do inspite increased excretion of your uric acid. 08:29 So, these are then known as uricosuric drugs. 08:32 These include your loop diuretics, such as probenecid and sulfunpyrazone. 08:38 Maybe uricase treatment, and there's a particular… keep this in mind, IL-1 β antagonist called anakinra.
About the Lecture
The lecture Tophaceous Gout by Carlo Raj, MD is from the course Introduction and Non-Autoimmune Arthritis. It contains the following chapters:
- Introduction to Tophaceous Gout
- Management of Gout
Included Quiz Questions
Which of the following conditions is caused by monosodium urate deposition in soft tissues?
- Tophaceous gout
- Raccoon eye
- Heberden nodes
- Bouchard nodes
- Erythema nodosum
Which of the following findings is most likely in the synovial fluid of a patient with gout?
- Negatively birefringent needle-shaped crystals under polarized light
- Positively birefringent needle-shaped crystals under nonpolarized light
- Negatively birefringent cubic crystals under nonpolarized light
- Rhomboid-shaped monosodium urate crystals
- Envelope-shaped monosodium urate crystals
What drug is most appropriate to prevent recurrent attacks of gout in patients with elevated uric acid levels?
- Allopurinol
- Prednisolone
- Indomethacin
- Ibubrofen
- Colchicine
Which of the following is the serum uric acid goal in the majority of patients with gout?
- Less than 6 mg/dL
- Less than 8 mg/dL
- Less than 9 mg/dL
- Less than 11 mg/dL
- Less than 5 mg/dL
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Possibly one of the best lectures on this platform! Dr. Raj truly is an amazing teacher, thank you for the lesson!
Comprehensive lecture, suitable for supplementing your studies. Overall good quality and good for reviewing your studies.