Playlist
Show Playlist
Hide Playlist
Non-ANCA-associated Small Vessel Vasculitides
-
I Rheumatology 05 Vasculitis.pdf
-
Download Lecture Overview
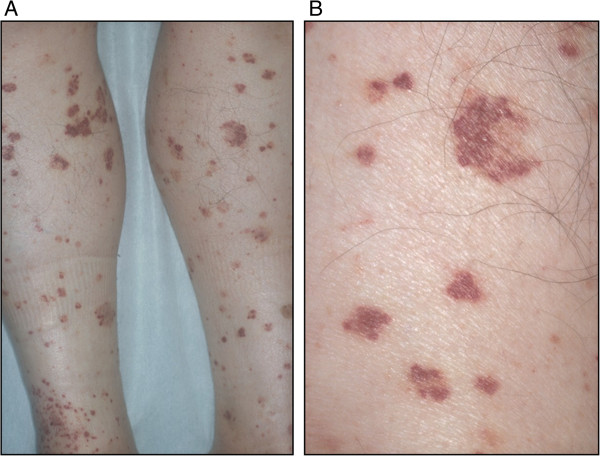
00:01 Here we’ll take a look at non-ANCA associated small vessel vasculitides. 00:04 We have now completed our discussion of those important ANCA-associated vasculitides. 00:10 So what do we mean by non-ANCA? Well these are pure immune involvement issues. 00:15 In other words, we’re talking about an immune complex that’s circulating throughout the body, circulating throughout the body causing damage to the endothelial cells and, therefore, resulting in purpura as being your major clinical manifestation. 00:34 What is the immunoglobulin that you find with Henoch-Schönlein purpura? Is it IgA, IgG or IgM? It is IgA. 00:46 Another name for Henoch-Schönlein purpura is IgA vasculopathy, which is what our topic is. It has nothing, I repeat—has nothing to do with ANCA. 00:57 Non-ANCA associated. 00:59 Who is your patient, clinically, walking through the door? A child. 01:03 Next, the momma says, “my child has a rash.” “Momma, tell me, where is this rash?” “Oh, it’s on the butt of my child and it’s on the lower extremities.” Now that the child is brought in, you as the clinician are checking for the signs of this purpura. 01:23 When you feel the lower extremity of the purpura, you can actually feel the bumps, called palpable purpura. This is anasarca purpura. 01:33 The palpable purpura, glomerulonephritis, now stop there for one second, let me make sure that I give you the significance of that. 01:41 Would you then call this Buerger? When you find—now please know this, be careful. 01:46 Some researches out there do not clearly distinguish between anasarca purpura and Buerger. Let me make sure that I make it clear for you. Here we go. 01:56 So when you have palpable purpura of the lower extremity of a child, #1 differential anasarca purpura. 02:03 What is the immunoglobulin to be affected or to be involved? IgA. 02:08 You do a biopsy of this rash, you’re going to find IgA. 02:12 Another name for anasarca purpura is IgA vasculopathy. 02:16 Is it possible that the immune complex may then travel through the blood vessels towards the kidney and cause ischemia and, therefore, cause glomerulonephritis? It could. Would you then call it Buerger? No, you would not. 02:30 So what is Buerger? Buerger is IgA nephropathy. 02:35 So that was a discussion that we had back in nephrology and so, therefore, in Buerger, it’s strictly IgA nephropathy in which IgA is then depositing in the mesangium without involvement of your blood vessels causing purpura. 02:50 So it has to be a clear distinction. 02:52 Otherwise, it’s impossible for you to choose the proper diagnosis. 02:59 So once you leave the kidney and you find significant palpable purpura, and then you think about anasarca purpura. 03:06 If that’s not clear, make sure that you repeat what I just said and not take this section in here of Henoch-Schönlein and also take a look at the section where I have discussed the very same with Buerger and Henoch in nephrology. 03:21 So now we have a child, lower extremity palpable purpura, maybe glomerulonephritis and the IgA could be found in the mesangium there as well. 03:29 So on immunofluorescence, clinically, the biopsy if required, clinically indistinguishable between the 2. 03:37 You could have issues with mesentery so therefore abdominal pain and look for arthritis. 03:42 That’s your clinical manifestation. 03:45 Diagnosis, as I said, you will then do a biopsy of the purpuric region and you will find which immunoglobulin? IgA. Commit that to memory. 03:55 Management: Self-limited, thank goodness, and short course of steroids might then be required for symptomatic relief. 04:05 Another condition is called cutaneous leukocytoclastic angiitis. 04:10 Here the skin lesions, purpura, are palpable. 04:14 Now most of the times when you have non-ANCA type of issues, it will be palpable purpura. Let me give you a differential here. 04:21 Usually secondary to drug reactions. 04:24 That is what your focus will be on. Cutaneous leukocytoclastic angiitis. 04:30 On immunofluorescence, testing the skin biopsy, you’ll find that leukocytoclastic vasculitis and your next step of management is remove the defending agent and a short course of corticosteroids. 04:45 I’d like to show you the hands of a patient with leukocytoclastic vasculitis, defending agent—the drugs, then causing a reaction. 04:54 The next type of management would then be to remove the defending agent whether it be antibiotics, chemotherapy, what have you, and then the symptoms of the patient would subside quite significantly. 05:07 We have another condition called essential mixed cryoglobulinemia. 05:11 It is a non-ANCA-associated vasculitis. What is this referring to? Immediately, your patient, most likely, history of hepatitis C. 05:20 Back in the ‘70s, there was an epidemic of hepatitis C. 05:24 Nowadays, we don’t have it as much but there’s still a large population of hepatitis C. 05:30 And with hepatitis C, we’re getting better, and actually incredibly successful at treating genotype 1. 05:37 And the drugs there that you must know from pharmacology in recent years, or actually in recent year is ledipasvir and sofosbuvir. 05:46 The combination of the 2 could be given, and within a 9-month period, could completely cure your patient of hepatitis C. 05:53 That’s something from pharmacology that you want to keep in mind. 05:56 Now the clinical manifestation, it’s an immune complex type of issue. 06:01 What do they mean complex? Causing damage to blood vessels, therefore, resulting in— no surprise—palpable purpura. 06:08 May also cause damage to the kidney—glomerulonephritis. 06:12 Will also have issues with the digits, mononeuritis multiplex and occasional hemoptysis. 06:17 Your focus here on hepatitis C clinical manifestation. 06:21 Your diagnostic studies. Looking for cryoglobulins. 06:25 The proteins that have now precipitated. 06:28 With the immune complex being activated, your [Inaudible 00:06:29] levels will drop, your C3 and C4. 06:33 Rheumatoid factor could be positive. 06:35 Hepatitis C particles usually present, but sometimes are absent during the flares as they are part of the cryocrit. 06:43 Management: Steroids. In cases associated with hepatitis C, these are some drugs that you want to keep in mind such as interferons and ribavirin, but as I told you, there are newer drugs out on the market and will be asked of you. 06:57 One will be ledipasvir and the other one would be sofosbuvir. 07:02 If I was you, I would research some of the newer drugs that are out there for a cure, specifically genotype 1 hepatitis C. 07:12 Severe cases—plasmapheresis is what you’re thinking to save your organs.
About the Lecture
The lecture Non-ANCA-associated Small Vessel Vasculitides by Carlo Raj, MD is from the course Vasculitis: Basic Principles with Carlo Raj.
Included Quiz Questions
A skin biopsy from a 5-year-old boy with a palpable purpuric rash on the lower extremities demonstrates predominantly IgA deposition. What is the most likely diagnosis?
- Henoch-Schonlein purpura
- Buerger disease
- Cutaneous leukocytoclastic angiitis
- Churg-Strauss syndrome
- Von Willebrand disease
Which of the following types of vasculitis is commonly associated with hepatitis C?
- Essential mixed cryoglobulinemia
- Henoch-Schonlein purpura
- Cutaneous leukocytoclastic angiitis
- Giant cell arteritis
- Granulomatosis with polyangiitis
What type of vasculitis secondary to drug reactions presents with purpuric skin lesions?
- Cutaneous leukocytoclastic angiitis
- Giant cell arteritis
- Granulomatosis with polyangiitis
- Henoch-Schonlein purpura
- Essential mixed cryoglobulinemia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
The lecture has been very clear and precise as it is often the case with Dr. Raj!