Playlist
Show Playlist
Hide Playlist
Respiratory Distress: Examination
-
Emergency Medicine Bord Respiratory Distress.pdf
-
Download Lecture Overview
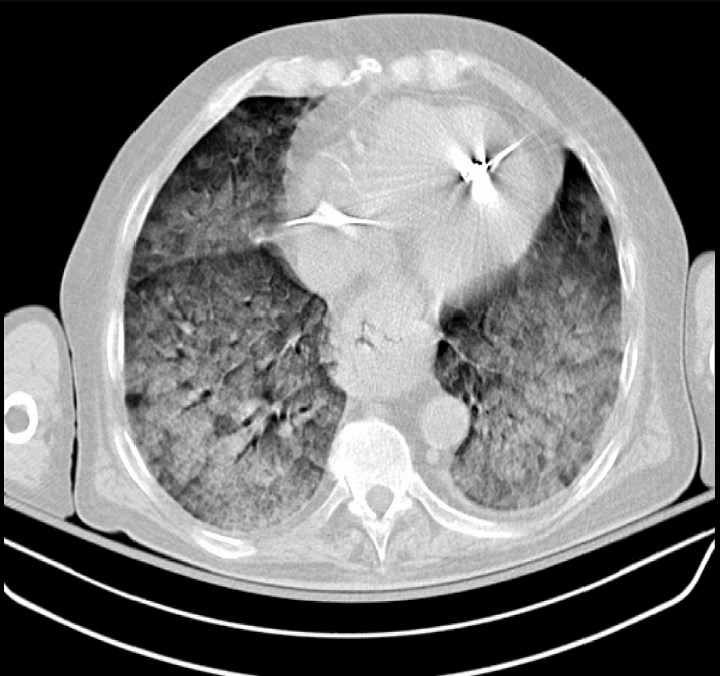
00:00 So when someone comes in in respiratory distress, the examination, you want to look at the patient. You can gather so much information just by looking at the patient from the door. You want to listen, you want to take a listen to your lungs. That can give you a clue as to what's going on with the patient. If you hear wheezing, that's potentially obstructive lung disease or asthma. If you hear rales or crackles, that's more likely to be CHF. And you want to go ahead and feel the patient's chest. You can do tactile fremitus and egophony. And the key thing in patients with respiratory distress is you're going to be treating them and examining them potentially all at the same time. So when someone comes in with severe respiratory distress, oftentimes our treatment and our exam and our history are all taking place at the same time because we're moving very quickly to rapidly treat and assess the patient. Now a key thing with respiratory distress is you always want to be reassessing your patient so you always want to be going back to your patient after you've given them a certain treatment, after you've given them nebulizer treatments or diuretics or started them on non-invasive ventilation and you always want to be going back and reassessing your patient. Your further physical exam, we want to focus on the respiratory rate. Oftentimes when someone is having significant respiratory distress, the respiratory rate will be elevated though sometimes you want to go ahead and you want to make sure you're focusing on that and that you're counting the respiratory rate and seeing what it is. Oftentimes, it will be obvious that the patient's respiratory rate is elevated. You want your patient to be on a pulse oximeter. You want to be able to measure their oxygen saturation and generally peripheral pulse oximeters are non invasive pulse oximeters do a pretty good job of measuring the patient's oxygenation. You also want to think about the patient's position. So oftentimes our instincts are for people to be lying flat in bed or flat on the stretcher, but for the most part if someone's in severe respiratory distress you want to sit them up in bed and the reason that you want to sit them up in bed is because when you're sitting up you're able to take deeper inhalations and you're able to recruit more of your lung volume. When you're lying down flat, you're not able to do that. The other thing that happens when you sit people up especially if they have some fluid in their lungs is the fluid goes to the bottom of their lungs and then they're able to utilize again larger portions of their lung volume and they're able to fill their lungs with more fluid. So gravity is your friend. Go ahead and sit those patients up. The fluid will go down, they're going to be able to breathe better in that situation. Lastly is listening and you want to definitely take a listen to the lungs, you want to see if you hear wheezes, if you hear crackles, if you hear crackles how far up those go, rhonchi or the other thing that you can sometimes hear, and all of those things will point you in a direction as to what you think is the most likely etiology of the shortness of breath for a patient. So in respiratory distress, the physical exam can provide you with lots of clues to the etiology of our patient's shortness of breath. Go ahead and utilize that exam, and much of that important information on the physical exam can actually be gathered in the first few seconds simply by walking in the room and looking at your patient. Looking at your patient, you could see if they're in respiratory distress. You can touch them very quickly and see if they're cool and clammy or if they're warm and red. 03:40 Also there's lots of information that you can just get in those first few seconds. Make sure that you utilize those first few moments to take a look at your patient. So like I said, in these situations we're going to be doing lots of step at the same time. We're going to be examining our patient, we're going to be intervening on their shortness of breath, we're going to be reassessing them, and then we're also going to be thinking about what initial tests we want to get. So we're going to start up by talking about some blood tests that you're going to want to get. When thinking about shortness of breath, we want to focus on the blood gas. 04:14 And when we're talking about a blood gas. For the most part in the emergency department, we utilize venous blood gases. Historically, we used to get arterial blood gasses. So we used to take blood from the artery and send that to the lab to analyze it. The advantage of taking an arterial blood gas over a venous blood gas is that an arterial gas can help you further assess the oxygenation. But like I said for the most part, our peripheral pulse oximeters that go on the patient's finger do a pretty good job of assessing the oxygenation. So for the most part in the ED, we sent a venous blood gas and the venous blood gas can take a pretty good look at the ventilation. So when we're talking about ventilation, we're talking about whether or not that person is able to adequately expire their carbon dioxide and when we're looking at a venous blood gas and our arterial blood gas they actually correlate pretty closely together. The other problem with an arterial blood gas is that can be challenging to get. For the most part, arterial blood gasses were obtained from the radial artery, which is the artery in the wrist. Now that historically can be painful for patients so we know that patients report a lot of pain with that procedure so generally we do the venous blood gas instead and we can just send the venous blood gas off with the rest of the labs that are sent off. We want to think about cardiac testing. So shortness of breath is sometimes due to problems in the lungs, but sometimes it's due to a problem with the heart so we want to think about sending off troponin testing. And then, other basic lab tests can give you additional information as well. 05:46 So, thinking about basic blood tests, you can find out if the patient is anemic. This anemia can cause shortness of breath. You can find out if there is kidney failure. The next step is thinking about imaging. So in imaging, we think about getting a chest x-ray. The chest x-ray can give you lots of information. It can take a look at the lung fields, you could see if there is a pneumonia and pneumothorax, if there's fluid in the lungs, and it can give you a lot of information about what's going inside the patient's lungs. However, additionally, if your chest x-ray is potentially not very revealing or you're not sure, you can move on and you can get a chest CT after you get some additional information. A chest CT scan gives you the advantage of taking a closer look at the patient's lung fields. The other thing that it can do is if you administer IV contrast with a chest CT, you can take a look at the vessels in the lungs and see if there's a blood clot there. An ultrasound scan of the lung can also be used in emergency settings to evaluate the pulmonary pleura and parenchyma. It can show signs of pleural effusion, consolidation, interstitial disease, and pneumothorax among other conditions. The lung ultrasound scan has additional advantages over chest x-rays and CT scans due to its availability, portability, absence of radiation, and real time application. Lastly, thinking about additional cardiac testing, the EKG is something that you can get that will look for ischemia. 07:16 So you can look and you could see if there is any evidence that the patient is having a heart attack or a myocardial infarction. You can also look for arrhythmias. Arrhythmia sometimes also can make people feel short of breath such as atrial fibrillation or atrial flutter, and then an echocardiogram. In the emergency department, we utilize bedside point of care ultrasound quite a lot and an echocardiogram is something that can be obtained easily and quickly. 07:41 Studies have shown that in the emergency department, emergency medicine physicians are good at figuring out if the patient has a good EF, a medium EF, or a low EF. So we're good at kind of approximating that and as technology just keeps getting better and where you are training our residents I think that this scale will only get utilized more and more over the upcoming years.
About the Lecture
The lecture Respiratory Distress: Examination by Sharon Bord, MD is from the course Respiratory Emergencies.
Included Quiz Questions
Which of the following statements on the evaluation of respiratory distress is NOT true?
- An invasive procedure is required to determine the patient's oxygenation.
- Many important pieces of information can be gathered in the first few seconds simply by looking at the patient.
- Auscultation of the lungs may help point to a possible etiology of a patient's shortness of breath.
- You must continue reassessing your patient with respiratory distress after every intervention.
- Significant respiratory distress will cause an elevated respiratory rate.
Which of the following statements regarding a blood gas evaluation is NOT true?
- Arterial blood gas is easier to acquire than venous blood gas.
- Venous blood gas evaluates ventilation.
- Arterial blood gas evaluates oxygenation.
- Venous blood gas correlates closely to arterial blood gas.
- Venous blood gas is preferred over arterial blood gas in the ED.
Which of the following is least likely to be diagnosed with a chest X-ray?
- Presence of Bronchiectasis
- Presence of pneumonia
- Presence of pneumothorax
- Presence of pleural fluid
- Atelectasis
Which of the following modalities may NOT be included in the initial evaluation of respiratory distress?
- Spirometry
- ECG
- Chest CT scan
- Chest x-ray
- Blood gases
Customer reviews
3,5 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
Very clear and concise. Presenter took time to explain positional importance of the patient.
1 customer review without text
1 user review without text