Playlist
Show Playlist
Hide Playlist
Anemia and Iron Deficiency – Red Cell Disorders
-
Slides Disorders of red cells.pdf
-
Download Lecture Overview
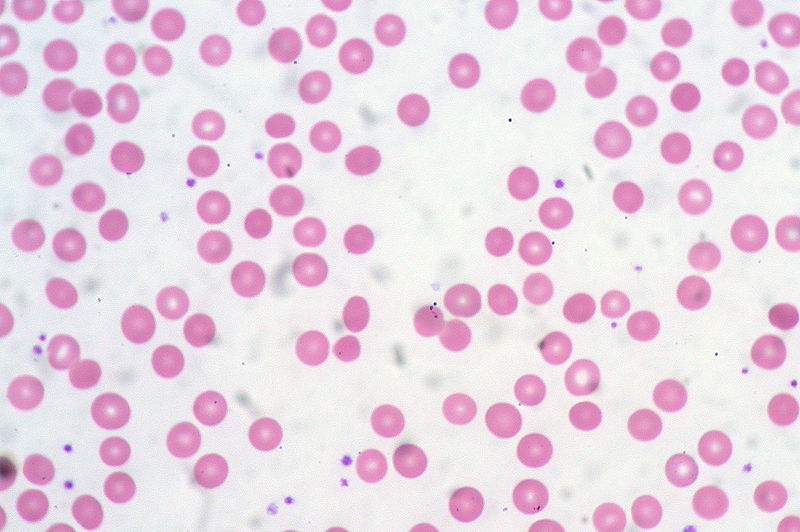
00:01 Hello, welcome to this lecture on disorders of the red cell. Learning outcomes that you will gain from this lecture include these four points. Red cell disorders are some of the most common diseases in the world. Anaemia can result from many different conditions such as iron deficiency, haemoglobinopathy and chronic infection. Haemolytic anaemia occurs when the red recall lifespan is reduced and increased numbers of red cells are seen in polycythemia, which may result from a myeloproliferative disease or response to hypoxia. 00:42 Let us start with the red cell itself and here is a very familiar electron micrograph of red cells showing a biconcave shape. Red cells derive from erythroblasts in the bone marrow. They are packed with haemoglobin and they carry oxygen deep into tissues. 01:05 The production of these cells is regulated by an erythropoietin and they do not have a nucleus, so their lifespan is limited and is around 120 days. Anaemia is very common throughout the world. 01:21 It can be defined as a reduction in the haemoglobin level within the blood, but remember that this must taken in relation to two factors. One is the age of the patient and the other is the gender. Let us look at that table on the right, which shows typical haemoglobin concentrations at different ages. If you look at the mean haemoglobin column, at birth cord blood has a high haemoglobin concentration around 165 g/L. Then the green line of one month shows this is already fallen to 140 g/L. In the first few weeks of life, there is a lot of breakdown of red cells within the blood and change of the globin to a different form. 02:14 At six months to 2 years, you will see a relatively a haemoglobin concentration, 120 g/L, which then starts to increase at the age of 12 to 18 to around 114. 02:31 Then look at adults right at the bottom and you will see the characteristic difference between females and males in haemoglobin concentration with males having an increment of around 15 g/L due to the fact on anabolic male hormones. Now the symptoms of anaemia include a range of things including tiredness, shortness of breath, poor concentration, palpitations because the heart is beating fast and vigorously and of course colour is a sign that somebody may be anaemic. A good method for approaching the classification of anaemia is through analysis of the red cell volume. So let us now take a look at that in a little more detail. 03:25 Here we see the classification of anaemia based on the mean cell volume. So, on the blue row, you will see the anaemia type, microcytic hypochromic. Those are small cells with low levels of haemoglobin. Here we have two subsets of disease that we will discuss in more detail, iron deficiency and thalassemia. In the middle, we have normal size cell, normocytic and normochromic. 03:56 These are due to chronic infection, renal disease and marrow disease and may also include haemolytic anaemia whereas on the right we have macrocytic anaemia, large red cells with a raised MCV. We will see later on how these are normally secondary to vitamin deficiency particularly vitamin B12 and folic deficiency. Let us take the first of these and that is an iron deficiency. First we have to consider the physiology of iron within your body. 04:33 Iron is one of the most common elements in the crust of the earth and yet we only have around 4 or 5 g of iron within our body. There is also no mechanism for regulating the excretion of iron and so we have to be very careful how much iron we absorb. We now think that this is the case because iron can be quite toxic in excess and it can even lead to damage of DNA and so the absorption of iron is controlled to levels that we just need to maintain normal physiological function. On the right, the diagram shows where this iron is held within the body and you will see that 70 percent is incorporated into haemoglobin with 25 percent stood in the reticuloendothelial system. Minor fractions are circulating within the blood. 05:36 This is a representation of iron regulation and we can see at the top our intake of iron is around 10 to 20 mg per day in our food. There are two major forms of iron that we encounter in our diet, heme iron comes in meat products and that is relatively well absorbed whereas nonheme iron is more tricky for our body to absorb. In the stomach, much of this iron is reduced into the ferrous Fe2+ form and that helps absorption and you will see that absorption occurs in the upper small intestine. But on the left-hand side of the slide, you will see much of this is absorbed into mucosal cells and then shed for excretion perhaps a milligram a day whereas around a mg goes into the blood stream and there is absorbed and is used in an erythropoiesis. So what is iron used for? It is used largely for making haemoglobin. Let us just look at how our cells make haemoglobin and you will see that is a representation of a mitochondrion on the left and at the top of the mitochondria, you will see glycine and succinyl CoA and those are the first derivatives that come together to form the constituents of the haem. The delta-ALA enzyme, aminolevulinic acid is a great limiting step here and it produces through intermediates protoporphyrin, which is very interesting flat planar molecule and you will see that comes out of the mitochondria links with iron and forms haem and of course haem needs globin and globin you see comes in the top right as amino acids forming these chains of 141 or 146 amino acids long. 07:51 As we bring haem and globin together, we form the haemoglobin, which is so densely concentrated within red cells. When we look later at haemolytic anaemias, we will take this process and reverse and see how haemoglobin is degraded and how they can lead to some of the symptoms of haemolytic anaemia. Iron deficiency is one of the most common findings in people around the globe and the major cause is chronic blood loss particularly through menstruation. 08:30 Women women who are premenopausal having regular menstruation are very commonly iron deficient. It can also be the result of gastro intestinal malignancy or inflammation. 08:44 That is very important because if you see a man who has iron deficiency anaemia clearly they cannot be menstruation that is a warning sign also in a postmenopausal woman. 08:59 You must think if there is a gastrointestinal cause perhaps a colonic tumour or even a gastric tumour. Those should be investigated in most cases. Dietary deficiency of iron is actually quite uncommon and malabsorption can occur and, of course, the celiac disease is an important consideration there, but they are relatively less common when actually chronic blood loss. 09:31 The treatment to iron deficiency is usually relatively easy and ends with an oral iron source, which should be around for over 100 years that is one of the cheapest tablets you can possibly buy. Now some people cannot tolerate oral iron. It can lead to some gastrointestinal upset and so intravenous iron can also be given and this is really very well tolerated now. Now on the right, there is a blood film of a person with iron deficiency and you can see how those cells fit those two criteria that we described microcytic that is more, hypochromic that polyhemoglobanised, you see very pale staining cells and another feature is pencil cells, very long thin cells as you can see in one or two places.
About the Lecture
The lecture Anemia and Iron Deficiency – Red Cell Disorders by Paul Moss, PhD, OBE, FMed, FRCPath is from the course Hematologic Disorders.
Included Quiz Questions
Which parameter measured on a a peripheral smear is used in the classification of anemia?
- Mean corpuscular volume
- Red cell hemoglobin
- Mean corpuscular hemoglobin concentration
- Red cell distribution width
- Mean hematocrit percentage
Where is most of the body's iron contained?
- Hemoglobin in RBC
- Ferritin in reticuloendothelial system
- Hemosiderin in reticuloendothelial system
- Transferrin in plasma
- Myoglobin in muscle
Which form of iron is most readily absorbed by the intestinal cells?
- Heme iron
- Ferric
- Transferrin
- Ferritin
- Hemosiderin
Which amino acid is involved in the synthesis of heme?
- Glycine
- Leucine
- Lysine
- Arginine
- Methionine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Thank you very much for easy and interesting interpretation of difficult topics