Playlist
Show Playlist
Hide Playlist
Histology of the Lung – Lung Anatomy
-
Slides 01 Respiratory Medicine Basics Brown.pdf
-
Download Lecture Overview
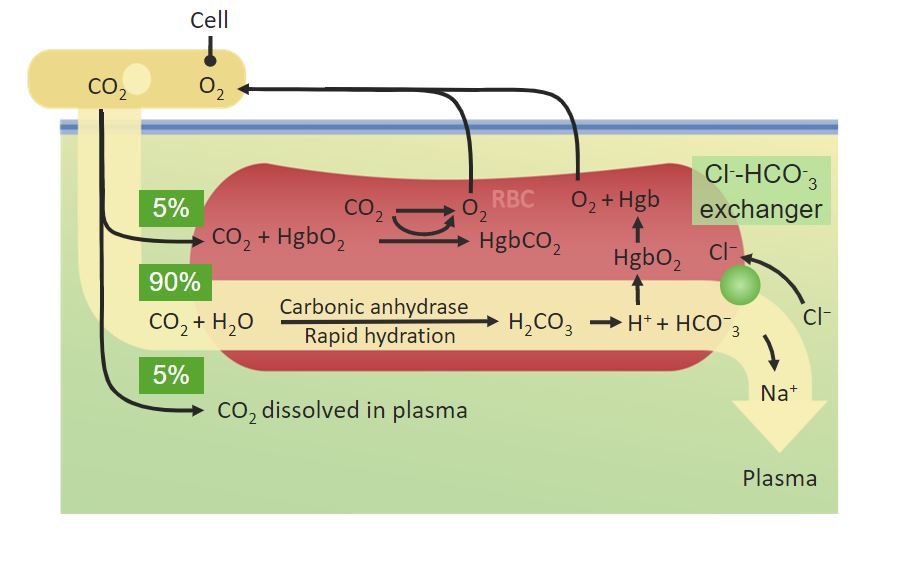
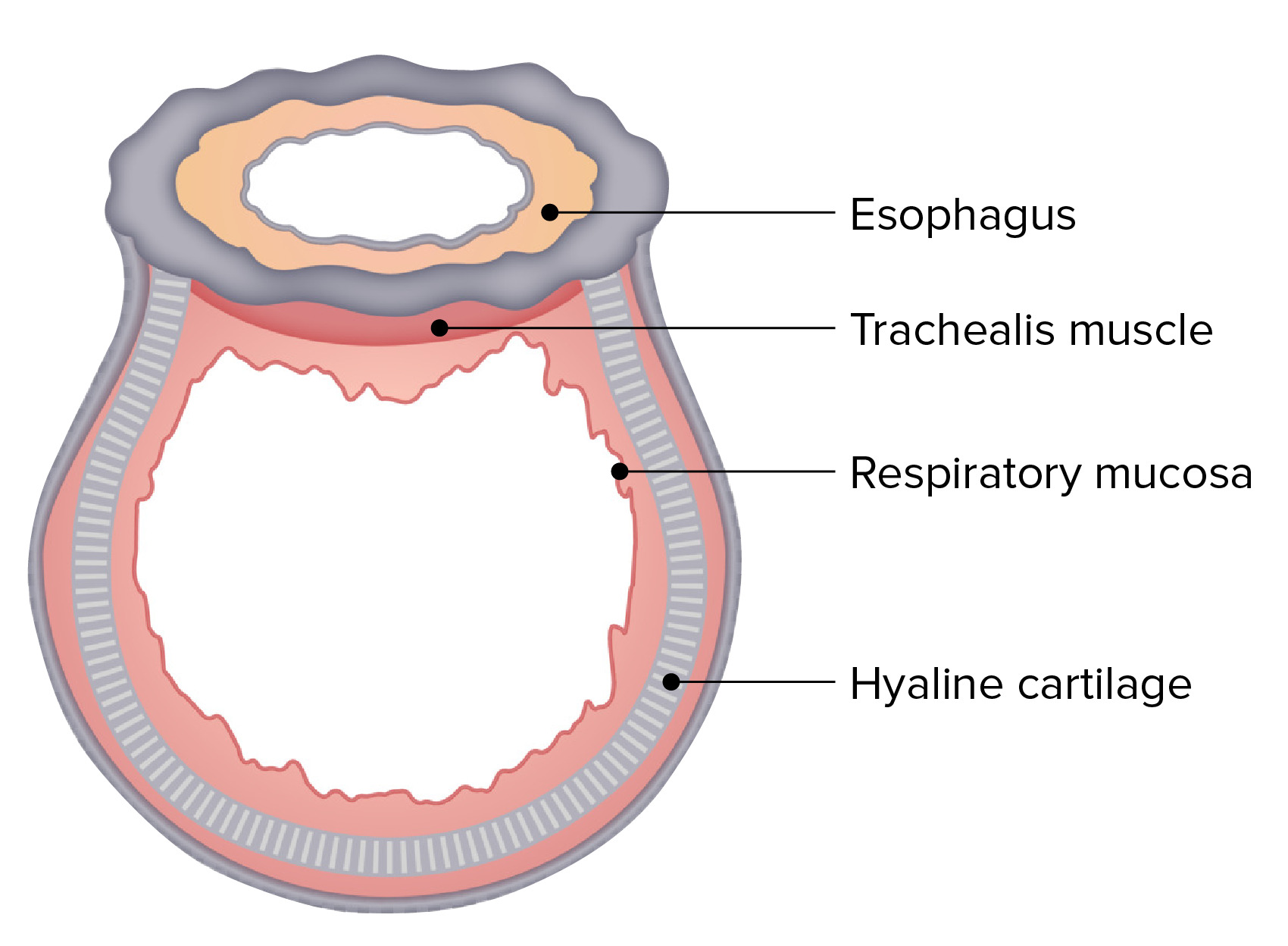
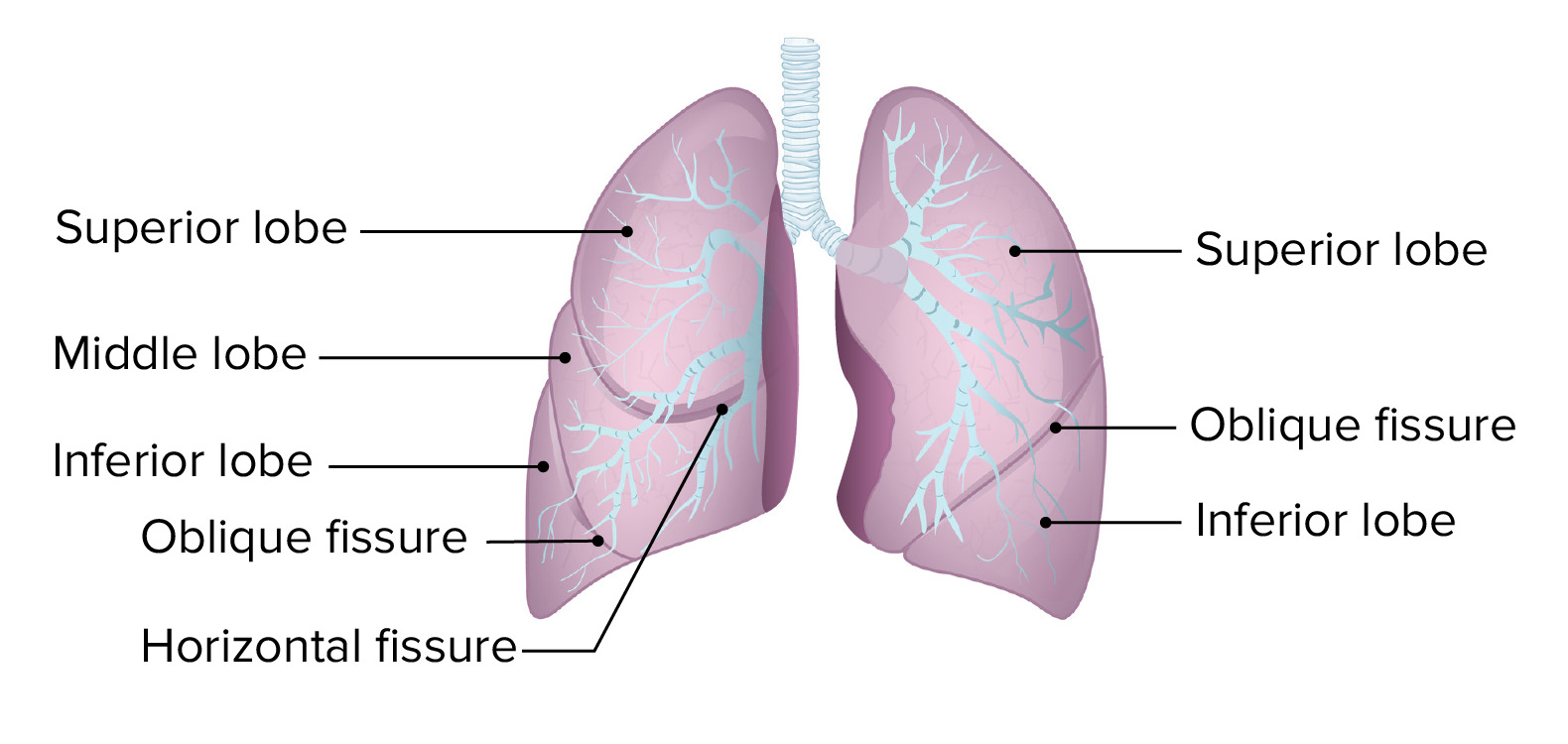
00:01 So what's the histology of the lung? If you get a microscope and look at the epithelium of the conducting airways, what does it look like? Well, largely, the conducting airways will have columnar epithelium, so that's a single layer of cells based on a basement membrane. There are oblong in shape. The nucleus tends to be at the base on the basement membrane, and then there'll be cilia projecting out the surface of the epithelial cell. And the cilia are protein structures which allow mucus to move back up the airways and out of the lungs, and that is a primary immune mechanism for defending the lung against anything that is inhaled that should not be there. 00:44 Underneath this layer of squamous epithelium, there will be various submucosal structures: a little bit of muscle around the main bronchi, some fibrocartilaginous layers, connective tissue, etc. Interspersed in the mucosal layer, there will be the occasional goblet cell, which produces mucus, and there are also submucosal glands which produce mucus, which are shown here in the middle part of this diagram, with an opening coming out into the epithelium from which mucus is secreted by the cells in the submucosa. As the airway goes… as you go down the airway towards the bronchioles, the amount of submucosa thins out, and the height of the columnar epithelium becomes smaller, and eventually, you'll lose your cilia as well. If you were to look at the alveolar epithelium in more detail, it'd look like this. There would be, as we described just now, an alveolus containing air. There's a type 1 pneumocyte there, you can see, which is forming a very large surface area of the alveolus. There's the occasional type 2 pneumocyte, with its synthetic function, and then in between alveoli, you can see, there's a small capillary with red cells in the middle and a filial cell forming a very thin capillary wall. And this is important, this structure, because of the small gap between the alveolus and the red cell in the capillary allows diffusion of oxygen from the alveoli into the red cells much more rapidly than it would be if there was a larger gap. The interstitium, which is in the middle, really is very thin in the lung and should remain so for good gas exchange. 02:31 I've mentioned already the visceral pleurae. So the pleurae are two layers which are consist of flattened squamous cell mesothelial cells—a single layer, a monolayer, which covers the underside of the thoracic cavity, so the ribs and the muscles of the parietal cavity of the parietal pleurae and the surface of the lung, the visceral pleurae, with a small gap between the two. Now that gap has a little bit of fluid in it in normal people, but it's a potential gap that can be filled up with air or filled up with fluid during disease situations. The visceral and the parietal pleurae merge at the hila, where there's a hole in the visceral pleurae created by this merging with the parietal pleurae that allows entry of the blood vessels and the right and the left main bronchi into the lungs. The nerve supply to the pleurae is from the intercostal nerves that we described earlier as lying underneath each rib. The nerve supply to the pleurae, which overlies the diaphragm, is from the phrenic nerve. So there is a pleural space, but it contains, in normal people, a minimal amount of fluid, acts as a sort of oil so that when you breathe, things can move nice and smoothly. The fluid forms from the bronchial intercostal circulation, so you get fluid oozing out from the lungs from the bronchial circulation and from the intercostal circulation but then drains down the lymphatics. And in general, that fluid formation and drainage is in balance, so the pleural space does not expand. But when you get disease that increases the amount of fluid coming out from the bronchial intercostal circulation (such as heart failure) or impairs the lymphatic drainage (if you've got abnormal pleurae, for example), then you may end up with pleural fluid forming in the pleural space and accumulating there to cause what we call a pleural effusion. 04:27 I've mentioned the hila already. This is a diagram showing them. So the gray part of the lung is covered in visceral pleura, and the gap where the visceral and the parietal pleurae fuse is right there in the middle of the medial aspect of each lung. And you can see the variety of blood vessels and airways that enter the lung and nerves at that point on either side.
About the Lecture
The lecture Histology of the Lung – Lung Anatomy by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Introduction to the Respiratory System.
Included Quiz Questions
Which of the following statements about the bronchial tree is CORRECT?
- The bronchi are lined with a single layer of ciliated columnar epithelium.
- The lingula is part of the right upper lobe.
- The bronchi are surrounded by bony rings.
- The bronchi are lined with a single layer of ciliated, cuboidal epithelium.
What is the function of the goblet cells?
- Mucus production
- Production of serous secretion
- Secretion of IgA
- Phagocytosis of pollutants
- Assist the immune response by secreting cytokines
While progressing downward along the bronchial tree, what changes occur in the structure of epithelial cells?
- The height of the columnar cells decreases.
- The number of mitochondria increases.
- The number of mitochondria decreases.
- The height of columnar cells increases.
- The cilia increase in length.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |